
| Home | Sources Directory | News Releases | Calendar | Articles | | Contact | |
Bipolar disorder
| Bipolar disorder | |
|---|---|
| Classification and external resources | |
 Many people involved with the arts, such as Vincent van Gogh, are believed to have suffered from bipolar disorder |
|
| ICD-10 | F31. |
| ICD-9 | 296.80 |
| OMIM | 125480 309200 |
| DiseasesDB | 7812 |
| MedlinePlus | 001528 |
| eMedicine | med/229 |
| MeSH | D001714 |
Bipolar disorder or manic-depressive disorder, which is also referred to as bipolar affective disorder or manic depression, is a psychiatric diagnosis that describes a category of mood disorders defined by the presence of one or more episodes of abnormally elevated energy levels, cognition, and mood with or without one or more depressive episodes. The elevated moods are clinically referred to as mania or, if milder, hypomania. Individuals who experience manic episodes also commonly experience depressive episodes, or symptoms, or mixed episodes in which features of both mania and depression are present at the same time.[1] These episodes are usually separated by periods of "normal" mood; but, in some individuals, depression and mania may rapidly alternate, which is known as rapid cycling. Extreme manic episodes can sometimes lead to such psychotic symptoms as delusions and hallucinations. The disorder has been subdivided into bipolar I, bipolar II, cyclothymia, and other types, based on the nature and severity of mood episodes experienced; the range is often described as the bipolar spectrum.
Data from the United States on lifetime prevalence varies; but it indicates a rate of around 1% for bipolar I, 0.5%'1% for bipolar II or cyclothymia, and 2%'5% for subthreshold cases meeting some, but not all, criteria. The onset of full symptoms generally occurs in late adolescence or young adulthood. Diagnosis is based on the person's self-reported experiences, as well as observed behavior. Episodes of abnormality are associated with distress and disruption and an elevated risk of suicide, especially during depressive episodes. In some cases, it can be a devastating long-lasting disorder. In others, it has also been associated with creativity, goal striving, and positive achievements. There is significant evidence to suggest that many people with creative talents have also suffered from some form of bipolar disorder.[2]
Genetic factors contribute substantially to the likelihood of developing bipolar disorder, and environmental factors are also implicated. Bipolar disorder is often treated with mood stabilizer medications and, sometimes, other psychiatric drugs. Psychotherapy also has a role, often when there has been some recovery of stability. In serious cases, in which there is a risk of harm to oneself or others, involuntary commitment may be used. These cases generally involve severe manic episodes with dangerous behavior or depressive episodes with suicidal ideation. There are widespread problems with social stigma, stereotypes, and prejudice against individuals with a diagnosis of bipolar disorder.[citation needed] People with bipolar disorder exhibiting psychotic symptoms can sometimes be misdiagnosed as having schizophrenia, another serious mental illness.[3]
The current term "bipolar disorder" is of fairly recent origin and refers to the cycling between high and low episodes (poles). A relationship between mania and melancholia had long been observed, although the basis of the current conceptualisation can be traced back to French psychiatrists in the 1850s. The term "manic-depressive illness" or psychosis was coined by German psychiatrist Emil Kraepelin in the late nineteenth century, originally referring to all kinds of mood disorder. German psychiatrist Karl Leonhard split the classification again in 1957, employing the terms unipolar disorder (major depressive disorder) and bipolar disorder.
Contents |
Signs and symptoms
Bipolar disorder is a condition in which people experience abnormally elevated (manic or hypomanic) and, in many cases, abnormally depressed states for periods of time in a way that interferes with functioning. Bipolar disorder has been estimated to afflict more than 5 million Americans'about 1 out of every 45 adults.[4] It is equally prevalent in men and women and is found across all cultures and ethnic groups.[5] Not everyone's symptoms are the same, and there is no simple physiological test to confirm the disorder. Bipolar disorder can appear to be unipolar depression. Diagnosing bipolar disorder is often difficult, even for mental health professionals. What distinguishes bipolar disorder from unipolar depression is that the affected person experiences states of mania and depression. Often bipolar is inconsistent among patients because some people feel depressed more often than not and experience little mania whereas others experience predominantly manic symptoms.
Depressive episode
Signs and symptoms of the depressive phase of bipolar disorder include persistent feelings of sadness, anxiety, guilt, anger, isolation, or hopelessness; disturbances in sleep and appetite; fatigue and loss of interest in usually enjoyable activities; problems concentrating; loneliness, self-loathing, apathy or indifference; depersonalization; loss of interest in sexual activity; shyness or social anxiety; irritability, chronic pain (with or without a known cause); lack of motivation; and morbid suicidal ideation.[6] In severe cases, the individual may become psychotic, a condition also known as severe bipolar depression with psychotic features.
Manic episode
Mania is the signature characteristic of bipolar disorder and, depending on its severity, is how the disorder is classified. Mania is generally characterized by a distinct period of an elevated, expansive, or irritable mood state. People commonly experience an increase in energy and a decreased need for sleep. A person's speech may be pressured, with thoughts experienced as racing. Attention span is low, and a person in a manic state may be easily distracted. Judgment may become impaired, and sufferers may go on spending sprees or engage in behavior that is quite abnormal for them. They may indulge in substance abuse, particularly alcohol or other depressants, cocaine or other stimulants, or sleeping pills. Their behavior may become aggressive, intolerant, or intrusive. People may feel out of control or unstoppable. People may feel they have been "chosen" and are "on a special mission" or have other grandiose or delusional ideas. Sexual drive may increase. At more extreme phases of bipolar I, a person in a manic state can begin to experience psychosis, or a break with reality, where thinking is affected along with mood.[7] Many people in a manic state experience severe anxiety and are very irritable (to the point of rage), while others are euphoric and grandiose.
To be diagnosed with mania according to the Diagnostic and Statistical Manual of Mental Disorders (DSM), a person must experience this state of elevated or irritable mood, as well as other symptoms, for at least one week, less if hospitalization is required.[8]
Hypomanic episode
Hypomania is generally a mild to moderate level of mania, characterized by optimism, pressure of speech and activity, and decreased need for sleep. Generally, hypomania does not inhibit functioning like mania[citation needed]. Many people with hypomania are actually in fact more productive than usual. Some people have increased creativity while others demonstrate poor judgment and irritability. Many people experience signature hypersexuality. These persons generally have increased energy and tend to become more active than usual. They do not, however, have delusions or hallucinations. Hypomania can be difficult to diagnose because it may masquerade as mere happiness, though it carries the same risks as mania.
Hypomania may feel good to the person who experiences it. Thus, even when family and friends learn to recognize the mood swings, the individual often will deny that anything is wrong.[9] What might be called a "hypomanic event", if not accompanied by complementary depressive episodes ("downs", etc.), is not typically deemed as problematic: The "problem" arises when mood changes are uncontrollable and, more importantly, volatile or "mercurial". If unaccompanied by depressive counterpart episodes or otherwise general irritability, this behavior is typically called hyperthymia, or happiness, which is, of course, perfectly normal. Indeed, the most elementary definition of bipolar disorder is an often "violent" or "jarring" state of essentially uncontrollable oscillation between hyperthymia and dysthymia.
Mixed affective episode
In the context of bipolar disorder, a mixed state is a condition during which symptoms of mania and clinical depression occur simultaneously (for example, agitation, anxiety, aggressiveness or belligerence, confusion, fatigue, impulsiveness, insomnia, irritability, morbid and/or suicidal ideation, panic, paranoia, persecutory delusions, pressured speech, racing thoughts, restlessness, and rage).[10]
Associated features
Associated features are clinical phenomena that often accompany the disorder but are not part of the diagnostic criteria for the disorder.
- Cognitive functioning
Reviews have indicated that most individuals diagnosed with bipolar disorder, but who are euthymic (not experiencing major depression or mania), do not show neuropsychological deficits on most tests.[11] Meta-analyses have indicated, by averaging the variable findings of many studies, cognitive deficits on some measures of sustained attention, executive function and verbal memory, in terms of group averages. On some tests, functioning is superior; however,[11] and sub-threshold mood states and psychiatric medications may account for some deficits.[12][13] A 2010 study found that "excellent performance" at school at age 15'16 was associated in males with a higher rate of developing bipolar disorder, but so was the poorest performance.[14] A 2005 study of young adult males found that poor performance on visuospatial tasks was associated with a higher rate of developing bipolar disorder, but so was high performance in arithmetic reasoning.[15]
- Creativity
Bipolar disorder has been associated with people involved in the arts but it is an ongoing question as to whether many creative geniuses had bipolar disorder.[16][17][18] Some studies have found a significant association between bipolar disorder and creativity, although it is unclear in which direction the cause lies or whether both conditions are caused by a third unknown factor; temperament has been hypothesized to be one such factor.[19][20][21]
- Goals
A series of authors have described mania or hypomania as being related to a high motivation to achieve, ambitious goal-setting, and sometimes high achievement. One study indicated that the pursuit of goals, encouraged by sometimes achieving them, can become emotionally dysregulated and involve the development of mania.[22] Individuals may have low self-esteem and difficulties in social adjustment, however, and by definition there are periods of depression with difficulty in motivation and functioning.[23]
Causes
The causes of bipolar disorder likely vary between individuals. Twin studies have been limited by relatively small sample sizes but have indicated a substantial genetic contribution, as well as environmental influence. For bipolar I, the (probandwise) concordance rates in modern studies have been consistently put at around 40% in monozygotic twins (same genes), compared to 0 to 10% in dizygotic twins.[24] A combination of bipolar I, II and cyclothymia produced concordance rates of 42% vs 11%, with a relatively lower ratio for bipolar II that likely reflects heterogeneity. The overall heritability of the bipolar spectrum has been put at 0.71.[25] There is overlap with unipolar depression and if this is also counted in the co-twin the concordance with bipolar disorder rises to 67% (Mz) and 19% (Dz).[26] The relatively low concordance between dizygotic twins brought up together suggests that shared family environmental effects are limited, although the ability to detect them has been limited by small sample sizes.[25]
Genetic
Genetic studies have suggested many chromosomal regions and candidate genes appearing to relate to the development of bipolar disorder, but the results are not consistent and often not replicated.[27] Although the first genetic linkage finding for mania was in 1969,[28] the linkage studies have been inconsistent.[29] (Genetic linkage studies may be followed by fine mapping searching for the phenomenon of linkage disequilibrium with a single gene, then DNA sequencing; using this approach causative DNA base pair changes have been reported for the genes P2RX7[30] and TPH1[citation needed]). Recent meta-analyses of linkage studies detected either no significant genome-wide findings or, using a different methodology, only two genome-wide significant peaks, on chromosome 6q and on 8q21. Genome-wide association studies have also not brought a consistent focus ' each has identified new loci, while none of the previously identified loci were replicated.[29] Findings did include a single-nucleotide polymorphism in DGKH;[31] a locus in a gene-rich region of high linkage disequilibrium (LD) on chromosome 16p12;[32] and a single-nucleotide polymorphism in MYO5B.[33] A comparison of these studies, combined with a new study, suggested an association with ANK3 and CACNA1C, thought to be related to calcium and sodium voltage-gated ion channels.[34] Diverse findings point strongly to heterogeneity, with different genes being implicated in different families.[35] Numerous specific studies find various specific links.[36][37][38][39][40] Advanced paternal age has been linked to a somewhat increased chance of bipolar disorder in offspring, consistent with a hypothesis of increased new genetic mutations.[41] A review seeking to identify the more consistent findings suggested several genes related to serotonin (SLC6A4 and TPH2), dopamine (DRD4 and SLC6A3), glutamate (DAOA and DTNBP1), and cell growth and/or maintenance pathways (NRG1, DISC1 and BDNF), although noting a high risk of false positives in the published literature. It was also suggested that individual genes are likely to have only a small effect and to be involved in some aspect related to the disorder (and a broad range of "normal" human behavior) rather than the disorder per se.[42]
Childhood precursors
Some limited long-term studies indicate that children who later receive a diagnosis of bipolar disorder may show subtle early traits such as subthreshold cyclical mood abnormalities, full major depressive episodes, and possibly ADHD with mood fluctuation. There may be hypersensitivity and irritability. There is some disagreement whether the experiences are necessarily fluctuating or may be chronic.[43] A history of stimulant use in childhood is found in high numbers of bipolar patients and has been found to cause an earlier onset of bipolar disorder and a worse clinical course, independent of attention deficit hyperactivity disorder.[44][45][46]
Life events and experiences
Evidence suggests that environmental factors play a significant role in the development and course of bipolar disorder, and that individual psychosocial variables may interact with genetic dispositions.[42] There is fairly consistent evidence from prospective studies that recent life events and interpersonal relationships contribute to the likelihood of onsets and recurrences of bipolar mood episodes, as they do for onsets and recurrences of unipolar depression.[47] There have been repeated findings that between a third and a half of adults diagnosed with bipolar disorder report traumatic/abusive experiences in childhood, which is associated on average with earlier onset, a worse course, and more co-occurring disorders such as PTSD.[48] The total number of reported stressful events in childhood is higher in those with an adult diagnosis of bipolar spectrum disorder compared to those without, particularly events stemming from a harsh environment rather than from the child's own behavior.[49] Early experiences of adversity and conflict are likely to make subsequent developmental challenges in adolescence more difficult, and are likely a potentiating factor in those at risk of developing bipolar disorder.[43]
Neural processes

Researchers hypothesize that abnormalities in the structure and/or function of certain brain circuits could underlie bipolar and other mood disorders. Some studies have found anatomical differences in areas such as the amygdala,[50] prefrontal cortex[51] and hippocampus. However, despite 25 years of research involving more than 7,000 MRI scans, studies continue to report conflicting findings and there remains considerable debate over the neuroscientific findings. Two fairly consistent abnormalities found in a meta-analysis of 98 MRI or CT neuroimaging studies were that groups with bipolar disorder had lateral ventricles which were on average 17% larger than control groups, and were 2.5 times more likely to have deep white matter hyperintensities. Given the size of the meta-analysis, it was concluded that the relatively small number of significant findings was perhaps surprising, and that there may be genuinely limited structural change in bipolar disorder, or perhaps heterogeneity has obscured other differences. In addition, it was noted that averaged associations found at the level of multiple studies may not exist for an individual.[52]
The "kindling" theory asserts that people who are genetically predisposed toward bipolar disorder can experience a series of stressful events,[53] each of which lowers the threshold at which mood changes occur. Eventually, a mood episode can start (and become recurrent) by itself. There is evidence of hypothalamic-pituitary-adrenal axis (HPA axis) abnormalities in bipolar disorder due to stress.[54]
Recent research in Japan hypothesizes that dysfunctional mitochondria in the brain may play a role [55]
Other recent research implicates issues with a sodium ATPase pump,[56] causing cyclical periods of poor neuron firing (depression) and hyper sensitive neuron firing (mania). This may only apply for type one, but type two apparently results from a large confluence of factors.[citation needed]
Melatonin activity
It has been suggested that a hypersensitivity of the melatonin receptors in the eye could be a reliable indicator of bipolar disorder, in studies called a trait marker, as it is not dependent on state (mood, time, etc.). In small studies, patients diagnosed as bipolar reliably showed a melatonin-receptor hypersensitivity to light during sleep, causing a rapid drop in sleeptime melatonin levels compared to controls.[57] Another study showed that drug-free, recovered, bipolar patients exhibited no hypersensitivity to light.[58] It has also been shown in humans that valproic acid, a mood stabilizer, increases transcription of melatonin receptors[59] and decreases eye melatonin-receptor sensitivity in healthy volunteers[60] while low-dose lithium, another mood stabilizer, in healthy volunteers, decreases sensitivity to light when sleeping, but doesn't alter melatonin synthesis.[61] The extent to which melatonin alterations may be a cause or effect of bipolar disorder are not fully known.
Psychological processes
Psychological studies of bipolar disorder have examined the development of a wide range of both the core symptoms of psychomotor activation and related clusterings of depression/anxiety, increased hedonic tone, irritability/aggression and sometimes psychosis. The existing evidence has been described as patchy in terms of quality but converging in a consistent manner. The findings suggest that the period leading up to mania is often characterized by depression and anxiety at first, with isolated sub-clinical symptoms of mania such as increased energy and racing thoughts. The latter increase and lead to increased activity levels, the more so if there is disruption in circadian rhythms or goal attainment events. There is some indication that once mania has begun to develop, social stressors, including criticism from significant others, can further contribute. There are also indications that individuals may hold certain beliefs about themselves, their internal states, and their social world (including striving to meet high standards despite it causing distress) that may make them vulnerable during changing mood states in the face of relevant life events. In addition, subtle frontal-temporal and subcortical difficulties in some individuals, related to planning, emotional regulation and attentional control, may play a role. Symptoms are often subthreshold and likely continuous with normal experience. Once (hypo)mania has developed, there is an overall increase in activation levels and impulsivity. Negative social reactions or advice may be taken less notice of, and a person may be more caught up in their own thoughts and interpretations, often along a theme of feeling criticised. There is some suggestion that the mood variation in bipolar disorder may not be cyclical as often assumed, nor completely random, but results from a complex interaction between internal and external variables unfolding over time; there is mixed evidence as to whether relevant life events are found more often in early than later episodes.[11] Many sufferers report inexplicably varied cyclical patterns, however.[62]
Diagnosis
Diagnosis is based on the self-reported experiences of an individual as well as abnormalities in behavior reported by family members, friends or co-workers, followed by secondary signs observed by a psychiatrist, nurse, social worker, clinical psychologist or other clinician in a clinical assessment. There are lists of criteria for someone to be so diagnosed. These depend on both the presence and duration of certain signs and symptoms. Assessment is usually done on an outpatient basis; admission to an inpatient facility is considered if there is a risk to oneself or others. The most widely used criteria for diagnosing bipolar disorder are from the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, the current version being DSM-IV-TR, and the World Health Organization's International Statistical Classification of Diseases and Related Health Problems, currently the ICD-10. The latter criteria are typically used in Europe and other regions while the DSM criteria are used in the USA and other regions, as well as prevailing in research studies.
An initial assessment may include a physical exam by a physician. Although there are no biological tests which confirm bipolar disorder, tests may be carried out to exclude medical illnesses such as hypo- or hyperthyroidism, metabolic disturbance, a systemic infection or chronic disease, and syphilis or HIV infection. An EEG may be used to exclude epilepsy, and a CT scan of the head to exclude brain lesions. Investigations are not generally repeated for relapse unless there is a specific medical indication.
There are several other mental disorders which may involve similar symptoms to bipolar disorder. These include schizophrenia,[63] schizoaffective disorder, drug intoxication, brief drug-induced psychosis, schizophreniform disorder and borderline personality disorder. Both borderline personality and bipolar disorder can involve what are referred to as "mood swings". In bipolar disorder, the term refers to the cyclic episodes of elevated and depressed mood which generally last weeks or months. The term in borderline personality refers to the marked lability and reactivity of mood, known as emotional dysregulation, due to response to external psychosocial and intrapsychic stressors; these may arise or subside suddenly and dramatically and last for seconds, minutes, hours or days. A bipolar depression is generally more pervasive with sleep, appetite disturbance and nonreactive mood, whereas the mood in dysthymia of borderline personality remains markedly reactive and sleep disturbance not acute.[64] Some hold that borderline personality disorder represents a subthreshold form of mood disorder,[65][66] while others maintain the distinctness, though noting they often coexist.[67][68]
Clinical scales
The Bipolar Spectrum Diagnostic Scale (BSDS)[69] was developed by Ronald Pies, MD and was later refined and tested by S. Nassir Ghaemi MD, MPH and colleagues. The BSDS arose from Pies's experience as a psychopharmacology consultant, where he was frequently called on to manage cases of "treatment-resistant depression". There are 19 question items and two sections on the English version of the BSDS. The scale was validated in its original version and demonstrated a high sensitivity.[70]
Criteria and subtypes
There is no clear consensus as to how many types of bipolar disorder exist.[71] In DSM-IV-TR and ICD-10, bipolar disorder is conceptualized as a spectrum of disorders occurring on a continuum. The DSM-IV-TR lists three specific subtypes and one for non-specified:[72]
- Bipolar I disorder
- One or more manic episodes. Subcategories specify whether there has been more than one episode, and the type of the most recent episode.[73] A depressive or hypomanic episode is not required for diagnosis, but it frequently occurs.
- Bipolar II disorder
- No manic episodes, but one or more hypomanic episodes and one or more major depressive episode.[74] However, a bipolar II diagnosis is not a guarantee that they will not eventually suffer from such an episode in the future.[citation needed] Hypomanic episodes do not go to the full extremes of mania (i.e., do not usually cause severe social or occupational impairment, and are without psychosis), and this can make bipolar II more difficult to diagnose, since the hypomanic episodes may simply appear as a period of successful high productivity and is reported less frequently than a distressing, crippling depression.
- Cyclothymia
- A history of hypomanic episodes with periods of depression that do not meet criteria for major depressive episodes.[75] There is a low-grade cycling of mood which appears to the observer as a personality trait, and interferes with functioning.
- Bipolar Disorder NOS (Not Otherwise Specified)
- This is a catchall category, diagnosed when the disorder does not fall within a specific subtype.[76] Bipolar NOS can still significantly impair and adversely affect the quality of life of the patient.
The bipolar I and II categories have specifiers that indicate the presentation and course of the disorder. For example, the "with full interepisode recovery" specifier applies if there was full remission between the two most recent episodes.[77]
Rapid cycling
Most people who meet criteria for bipolar disorder experience a number of episodes, on average 0.4 to 0.7 per year, lasting three to six months.[78][79]
Rapid cycling, however, is a course specifier that may be applied to any of the above subtypes. It is defined as having four or more episodes per year and is found in a significant fraction of individuals with bipolar disorder. The definition of rapid cycling most frequently cited in the literature (including the DSM) is that of Dunner and Fieve: at least four major depressive, manic, hypomanic or mixed episodes are required to have occurred during a 12-month period.[80] There are references that describe very rapid (ultra-rapid) or extremely rapid[81] (ultra-ultra or ultradian) cycling. One definition of ultra-ultra rapid cycling is defining distinct shifts in mood within a 24-to-48-hour period.
Challenges
The experiences and behaviors involved in bipolar disorder are often not understood by individuals or recognized by mental health professionals, so diagnosis may sometimes be delayed for 10 years or more.[82] That treatment lag is apparently not decreasing, even though there is now increased public awareness of this mental health condition in popular magazines and health websites. Despite this increased focus, individuals are still commonly misdiagnosed.[83] An individual may appear simply depressed when they are seen by a health professional. This can result in misdiagnosis of Major Depressive Disorder and harmful treatments. Screening tools such as the Hypomanic Check List Questionnaire (HCL-32)[84] have been developed to assist the quite often difficult detection of bipolar II disorders.
However, there is also a long-standing issue in the research literature as to whether a categorical classificatory divide between unipolar and bipolar depression is actually valid, or whether it is more accurate to talk of a continuum involving dimensions of depression and mania.[85][86]
It has been noted that the bipolar disorder diagnosis is officially characterised in historical terms such that, technically, anyone with a history of (hypo)mania and depression has bipolar disorder whatever their current or future functioning and vulnerability. This has been described as "an ethical and methodological issue", as it means no one can be considered as being recovered (only "in remission") from bipolar disorder according to the official criteria. This is considered especially problematic given that brief hypomanic episodes are widespread among people generally and not necessarily associated with dysfunction.[11]
Flux is the fundamental nature of bipolar disorder.[87] Individuals with the illness have continual changes in energy, mood, thought, sleep, and activity. The diagnostic subtypes of bipolar disorder are thus static descriptions'snapshots, perhaps'of an illness in continual flux, with a great diversity of symptoms and varying degrees of severity. Individuals may stay in one subtype, or change into another, over the course of their illness.[88] The DSM-V, to be published in 2013, will likely include further and more accurate sub-typing (Akiskal and Ghaemi, 2006).
The diagnosis of bipolar disorder can be complicated by coexisting psychiatric conditions such as obsessive-compulsive disorder, social phobia, panic disorder, or attention-deficit/hyperactivity disorder. Substance abuse may predate the appearance of bipolar symptoms, further complicating the diagnosis. A careful longitudinal analysis of symptoms and episodes, enriched if possible by discussions with friends and family members, is crucial to establishing a valid treatment plan where these comorbidities exist.[89]
The diagnosis of bipolar disorder in children is particularly challenging, and controversial. Some who show some bipolar symptoms tend to have a rapid-cycling or mixed-cycling pattern that may not meet DSM-IV criteria.[90] In addition, it can be difficult to distinguish between age-appropriate restlessness, the fidgeting of children with ADHD, and the purposeful busy activity of mania.[91] Further complicating the diagnosis, is that abused or traumatized children can seem to have bipolar disorder when they are actually reacting to horrors in their lives.[92]
In the elderly, recognition and treatment of bipolar disorder may be complicated by the presence of dementia or the side effects of medications being taken for other conditions.[93] As yet there is very little evidence-based research to guide management of bipolar in the elderly as opposed to adults in general.
Management
There are a number of pharmacological and psychotherapeutic techniques used to treat Bipolar Disorder. Individuals may use self-help and pursue a personal recovery journey.
Hospitalization may be required especially with the manic episodes present in bipolar I. This can be voluntary or (if mental health legislation allows and varying state-to-state regulations in the USA) involuntary (called civil or involuntary commitment). Long-term inpatient stays are now less common due to deinstitutionalization, although can still occur.[94] Following (or in lieu of) a hospital admission, support services available can include drop-in centers, visits from members of a community mental health team or Assertive Community Treatment team, supported employment and patient-led support groups, intensive outpatient programs. These are sometimes referred to partial-inpatient programs.[95]
Psychosocial
Psychotherapy is aimed at alleviating core symptoms, recognizing episode triggers, reducing negative expressed emotion in relationships, recognizing prodromal symptoms before full-blown recurrence, and, practicing the factors that lead to maintenance of remission[96] Cognitive behavioural therapy, family-focused therapy, and psychoeducation have the most evidence for efficacy in regard to relapse prevention, while interpersonal and social rhythm therapy and cognitive-behavioural therapy appear the most effective in regard to residual depressive symptoms. Most studies have been based only on bipolar I, however, and treatment during the acute phase can be a particular challenge.[97] Some clinicians emphasize the need to talk with individuals experiencing mania, to develop a therapeutic alliance in support of recovery.[98]
Medication
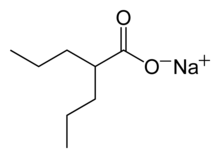
The mainstay of treatment is a mood stabilizer medication such as lithium carbonate or lamotrigine.[99][100] Lamotrigine has been found to be best for preventing depressions, while lithium is the only drug proven to reduce suicide in bipolar patients. These two drugs comprise several unrelated compounds which have been shown to be effective in preventing relapses of manic, or in the one case, depressive episodes. The first known and "gold standard" mood stabilizer is lithium,[101] while almost as widely used is sodium valproate,[102] also used as an anticonvulsant. Other anticonvulsants used in bipolar disorder include carbamazepine, reportedly more effective in rapid cycling bipolar disorder, and lamotrigine, which is the first anticonvulsant shown to be of benefit in bipolar depression.[103]
Treatment of the agitation in acute manic episodes has often required the use of atypical antipsychotic medications, such as quetiapine, olanzapine and chlorpromazine. More recently, olanzapine and quetiapine have been approved as effective monotherapy for the maintenance of bipolar disorder.[104] A head-to-head randomized control trial in 2005 has also shown olanzapine monotherapy to be as effective and safe as lithium in prophylaxis.[105]
The use of antidepressants in bipolar disorder has been debated, with some studies reporting a worse outcome with their use triggering manic, hypomanic or mixed episodes, especially if no mood stabiliser is used. However, most mood stabilizers are of limited effectiveness in depressive episodes. Rapid cycling can be induced or made worse by antidepressants, unless there is adjunctive treatment with a mood stabilizer.[106][107] One large-scale study found that depression in bipolar disorder responds no better to an antidepressant with mood stabilizer than it does to a mood stabilizer alone.[108] Recent research indicates that triacetyluridine may help improve symptoms of bipolar disorder.[109] Clinical studies have shown that Omega 3 fatty acids may have beneficial effects on bipolar disorder.[110]
Also, topiramate is an anticonvulsant often prescribed as a mood stabilizer. It is an off-label use when used to treat bipolar disorder. Unfortunately, its usefulness is likely minimal and side effects, such as significant cognitive impairment, undermine its efficacy (Kushner, et al. 2006 Bipolar Disorders 8; Chengappa, et al. 2006 J Clin Psych; 6).
When medication causes a reduction in symptoms or complete remission, it is important for someone with a bipolar disorder to understand they should continue to take the medicine. This can be complicated, as effective treatment may result in the reduction of manic symptoms and/or the medicine can be mood blunting or sedative, resulting in the person feeling they are stifled or that the medicine isn't working. Either way, relapse is likely to occur if the medicine is discontinued.
Prognosis
For many individuals with bipolar disorder a good prognosis results from good treatment, which, in turn, results from an accurate diagnosis. Because bipolar disorder can have a high rate of both under-diagnosis and misdiagnosis[citation needed], it is often difficult for individuals with the condition to receive timely and competent treatment.
Bipolar disorder can be a severely disabling medical condition. However, many individuals with bipolar disorder can live full and satisfying lives. Quite often, medication is needed to enable this. Persons with bipolar disorder may have periods of normal or near normal functioning between episodes.[111]
Ultimately one's prognosis depends on many factors, several of which are within the control of the individual. Such factors may include: the right medicines, with the right dose of each; comprehensive knowledge of the disease and its effects; a positive relationship with a competent medical doctor and therapist; and good physical health, which includes exercise, nutrition, and a regulated stress level.
There are obviously other factors that lead to a good prognosis as well, such as being very aware of small changes in one's energy, mood, sleep and eating behaviors, as well as having a plan in conjunction with one's doctor for how to manage subtle changes that might indicate the beginning of a mood swing. Some people find that keeping a log of their moods can assist them in predicting changes.[112]
Functioning
A recent 20-year prospective study on bipolar I and II found that functioning varied over time along a spectrum from good to fair to poor. During periods of major depression or mania (in BPI), functioning was on average poor, with depression being more persistently associated with disability than mania. Functioning between episodes was on average good ' more or less normal. Subthreshold symptoms were generally still substantially impairing, however, except for hypomania (below or above threshold) which was associated with improved functioning.[113]
Another study confirmed the seriousness of the disorder as "the standardized all-cause mortality ratio among patients with BD is increased approximately two-fold." Bipolar disorder is currently regarded "as possibly the most costly category of mental disorders in the United States." Episodes of abnormality are associated with distress and disruption, and an elevated risk of suicide, especially during depressive episodes.[114]
Recovery
A naturalistic study from first admission for mania or mixed episode (representing the hospitalized and therefore most severe cases) found that 50% achieved syndromal recovery (no longer meeting criteria for the diagnosis) within six weeks and 98% within two years. 72% achieved symptomatic recovery (no symptoms at all) and 43% achieved functional recovery (regaining of prior occupational and residential status). However, 40% went on to experience a new episode of mania or depression within 2 years of syndromal recovery, and 19% switched phases without recovery.[115] Many therapists treat individuals with bipolar I and II by helping them identify the return of symptoms, and actions that will prevent symptoms from getting worse.[116]
Recurrence
The following behaviors can lead to depressive or manic recurrence:[citation needed]
- Discontinuing or lowering one's dose of medication.
- Being under- or over-medicated. Generally, taking a lower dosage of a mood stabilizer can lead to relapse into mania. Taking a lower dosage of an antidepressant may cause the patient to relapse into depression, while higher doses can cause destabilization into mixed-states or mania.
- An inconsistent sleep schedule can aggravate symptoms. Too much sleep can be an indicator that depression is returning. It has been found that too little sleep can lead to mixed states/mania.
- Caffeine can cause destabilization of mood toward irritability, dysphoria, and mania. Anecdotal evidence seems to suggest that lower dosages of caffeine can have effects ranging from anti-depressant to mania-inducing.
- Inadequate stress management and poor lifestyle choices. If unmedicated, excessive stress can cause the individual to relapse. Medication raises the stress threshold somewhat, but too much stress still causes relapse.
- Often bipolar individuals are subject to self-medication, the most common drugs being alcohol, diazepam/sleeping tablets and marijuana. Studies show that tobacco smoking induces a calming effect on most bipolar people. A very high percentage of bipolar people may smoke for this reason.[117]
Recurrence can be managed by the sufferer with the help of a close friend, based on the occurrence of idiosyncratic prodromal events.[118] This theorizes that a close friend could notice which moods, activities, behaviours, thinking processes, or thoughts typically occur at the outset of bipolar episodes. They can then take planned steps to slow or reverse the onset of illness, or take action to prevent the episode from being damaging.[119]
Morbidity
According to an article in Psychiatric Times by McIntyre et al.,
-
- "Mortality studies have documented an increase in all-cause mortality in patients with BD (Bipolar Disorder). A newly established and rapidly growing database indicates that mortality due to chronic medical disorders (eg, cardiovascular disease) is the single largest cause of premature and excess deaths in BD. The standardized mortality ratio from suicide in BD is estimated to be approximately 18 to 25, further emphasizing the lethality of the disorder."[120]
Most people with bipolar disorder never attempt suicide or complete it. The annual average suicide rate in males and females with diagnosed bipolar disorder is 0.4%. This is 10 to more than 20 times that of the general population.[121]
Bipolar disorder can cause suicidal ideation that leads to suicidal, especially during mixed states such as dysphoric mania and agitated depression.[122] Persons suffering from bipolar II have high rates of suicide compared to persons suffering from other mental health conditions, including Major Depression. Major Depressive episodes are part of the bipolar II experience, and there is evidence that sufferers of this disorder spend proportionally much more of their life in the depressive phase of the illness than their counterparts with bipolar I Disorder (Akiskal & Kessler, 2007[which?]).
Epidemiology

The lifetime prevalence of bipolar disorder type I, which includes at least a lifetime manic episode, has generally been estimated at 2%.[123] A reanalysis of data from the National Epidemiological Catchment Area survey in the United States, however, suggested that 0.8 percent experience a manic episode at least once (the diagnostic threshold for bipolar I) and 0.5 a hypomanic episode (the diagnostic threshold for bipolar II or cyclothymia). Including sub-threshold diagnostic criteria, such as one or two symptoms over a short time-period, an additional 5.1 percent of the population, adding up to a total of 6.4 percent, were classed as having a bipolar spectrum disorder.[124] A more recent analysis of data from a second US National Comorbidity Survey found that 1% met lifetime prevalence criteria for bipolar 1, 1.1% for bipolar II, and 2.4% for subthreshold symptoms.[125] There are conceptual and methodological limitations and variations in the findings. Prevalence studies of bipolar disorder are typically carried out by lay interviewers who follow fully structured/fixed interview schemes; responses to single items from such interviews may suffer limited validity. In addition, diagnosis and prevalence rates are dependent on whether a categorical or spectrum approach is used. Concerns have arisen about the potential for both underdiagnosis and overdiagnosis.[126]
Late adolescence and early adulthood are peak years for the onset of bipolar disorder.[127][128] These are critical periods in a young adult's social and vocational development, and they can be severely disrupted.
Major depressive disorder and bipolar disorder are currently classified as separate disorders. Some researchers increasingly view them as part of an overlapping spectrum that also includes anxiety and psychosis. According to Hagop Akiskal, M.D., at the one end of the spectrum is bipolar type schizoaffective disorder, and at the other end is recurrent unipolar depression, with the anxiety disorders present across the spectrum. Also included in this view is premenstrual dysphoric disorder, postpartum depression, and postpartum psychosis. This view helps to explain why many people who have the illness do not have first-degree relatives with clear-cut "bipolar disorder", but who have family members with a history of these other disorders.
Children
In professional classifications such as the American Psychiatric Association's Diagnostic and Statistical Manual (DSM) [129] or the World Health Organization's International Classification of Diseases (ICD)[130] bipolar disorder is classified with adult onset disorders. However, as far back as the 1920s, Kraepelin [131] showed in a retrospective study of 900 manic-depressive adults that 0.4% had onset of symptoms before the age of ten. In a cohort of bipolar disordered adults, Loranger and Levine [132] retrospectively evaluated 200 adult bipolar patients and found that 0.5% had onset between the ages of five and nine. In a study of 898 adults with bipolar disorder, Goodwin and Jamison [133] found that 0.3% had onset before age 10. This literature supported the existence of childhood onset mania, but also indicated that it may be rare.
This idea was supported by a review of 28 papers by Anthony and Scott,[134] which suggested that childhood bipolar disorder was uncommon. In these papers, only three of 60 cases (5%) of purported childhood bipolar disorder met their criteria for bipolar disorder. However, Anthony and Scott's criteria differed from those currently in use, so the applicability of this work to current views of bipolar disorder is uncertain.
Population and community studies using DSM criteria show that about 1% of youth may have bipolar disorder.[135][136] Studies in clinics using these criteria show that up to 20% of youth referred to psychiatric clinics have bipolar disorder.[137][138][139] Many of these children required hospitalization due to the severity of their disorder [140][141]
Because of these diagnostic uncertainties, the validity of an early-onset form of bipolar disorder had been debated in the late 20th century. However, since that time, systematic reviews of diagnostic, genetic, neurobiological, treatment and longitudinal research studies [142][143][144][145] have concluded that this disorder can be validly diagnosed in children and adolescents. This consensus of the scientific community is also seen in the appearance of practice parameters for the disorder from the American Academy of Child and Adolescent Psychiatry[146]
Findings indicate that the number of American [children] and [adolescents] treated for bipolar disorder increased 40-fold from 1994 to 2003, and continues to increase. The data suggest that doctors had been more aggressively applying the diagnosis to children, rather than that the incidence of the disorder has increased. The study calculated the number of psychiatric visits increased from 20,000 in 1994 to 800,000 in 2003, or 1% of the [population] under age 20.[147]
The reasons for this increase in diagnosis are unclear. On the one hand, the recent consensus from the scientific community (see above) will have educated clinicians about the nature of the disorder and the methods for diagnosis and treatment in children. That, in turn, should increase the rate of diagnosis. On the other hand, assumptions regarding behavior, particularly in regard to the differential diagnosis of bipolar disorder, ADHD, and conduct disorder in children and adolescents, may also play a role.
Another factor is that the "consensus" regarding the diagnosis in the pediatric age group seems to apply only to the USA. The British National Institute on Health and Clinical Excellence (NICE) guidelines on bipolar disorder in 2006 [148] specifically described the broadened criteria used in the USA to diagnose bipolar disorder in children as suitable "only for research" and "were not convinced that evidence currently exists to support the everyday clinical use of (pediatric bipolar phenotype) diagnoses" which increase the "risk that medicines may be used to inappropriately treat a bipolar diathesis that does not exist."(p526). A 2002 German survey [149] of 251 child and adolescent psychiatrists (average 15 years clinical experience), found only 8% had ever diagnosed a pre-pubertal case of bipolar disorder in their careers. A similar survey of 199 child and adolescent psychiatrists (av 15 years clinical experience) in Australia and New Zealand [150] also found much lower rates of diagnosis than in the USA and a consensus that bipolar disorder was overdiagnosed in children and youth in the USA. Concerns about overdiagnosis in the USA have also been expressed by American child & adolescent psychiatrists [151][152][153][154] and a series of essays in the book "Bipolar children: Cutting-edge controversy, insights and research" [155] highlight several controversies and suggest the science still lacks consensus with regard to bipolar disorder diagnosis in the pediatric age group.
Although accurately diagnosing all disorders in children is important, for bipolar disorder, it is critical. On the one hand, the antipsychotic drugs sometimes prescribed for the treatment of bipolar disorder may increase risk to health including heart problems, diabetes, liver failure, and death.[156] On the other hand, bipolar disorder is a very disabling disorder which leads to many impairments in children, including cognitive impairment,[157][158][159] psychiatric hospitalization,[138][139][160][161][162] psychosis [138][139][161][162] and suicide.[163] Thus, physicians, parents and patients need to weight the potential risks and benefits when treating this disorder.[164]
Older age
There is a relative lack of knowledge about bipolar disorder in late life. There is evidence that it becomes less prevalent with age but nevertheless accounts for a similar percentage of psychiatric admissions; that older bipolar patients had first experienced symptoms at a later age; that later onset of mania is associated with more neurologic impairment; that substance abuse is considerably less common in older groups; and that there is probably a greater degree of variation in presentation and course, for instance individuals may develop new-onset mania associated with vascular changes, or become manic only after recurrent depressive episodes, or may have been diagnosed with bipolar disorder at an early age and still meet criteria. There is also some weak evidence that mania is less intense and there is a higher prevalence of mixed episodes, although there may be a reduced response to treatment. Overall there are likely more similarities than differences from younger adults.[165]
History
Variations in moods and energy levels have been observed as part of the human experience since time immemorial. The words "melancholia" (an old word for depression) and "mania" have their etymologies in Ancient Greek. The word melancholia is derived from melas/î�î�î»î�ς, meaning "black", and chole/χî¿î»î�, meaning "bile" or "gall",[166] indicative of the term's origins in pre-Hippocratic humoral theories. Within the humoral theories, mania was viewed as arising from an excess of yellow bile, or a mixture of black and yellow bile. The linguistic origins of mania, however, are not so clear-cut. Several etymologies are proposed by the Roman physician Caelius Aurelianus, including the Greek word 'ania', meaning to produce great mental anguish, and 'manos', meaning relaxed or loose, which would contextually approximate to an excessive relaxing of the mind or soul (Angst and Marneros 2001). There are at least five other candidates, and part of the confusion surrounding the exact etymology of the word mania is its varied usage in the pre-Hippocratic poetry and mythologies (Angst and Marneros 2001).
The basis of the current conceptualisation of manic-depressive illness can be traced back to the 1850s; on January 31, 1854, Jules Baillarger described to the French Imperial Academy of Medicine a biphasic mental illness causing recurrent oscillations between mania and depression, which he termed folie à double forme ('dual-form insanity').[167] Two weeks later, on February 14, 1854, Jean-Pierre Falret presented a description to the Academy on what was essentially the same disorder, and designated folie circulaire ('circular insanity') by him.(Sedler 1983) The two bitterly disputed as to who had been the first to conceptualise the condition.
These concepts were developed by the German psychiatrist Emil Kraepelin (1856'1926), who, using Kahlbaum's concept of cyclothymia,[168] categorized and studied the natural course of untreated bipolar patients. He coined the term manic depressive psychosis, after noting that periods of acute illness, manic or depressive, were generally punctuated by relatively symptom-free intervals where the patient was able to function normally.[169]
The term "manic-depressive reaction" appeared in the first American Psychiatric Association Diagnostic Manual in 1952, influenced by the legacy of Adolf Meyer who had introduced the paradigm illness as a reaction of biogenetic factors to psychological and social influences.[170] Subclassification of bipolar disorder was first proposed by German psychiatrist Karl Leonhard in 1957; he was also the first to introduce the terms bipolar (for those with mania) and unipolar (for those with depressive episodes only).[171]
Society and culture
Cultural references
Kay Redfield Jamison, a clinical psychologist and Professor of Psychiatry at the Johns Hopkins University School of Medicine, profiled her own bipolar disorder in her memoir An Unquiet Mind (1995).[172] In her book, Touched with Fire (1993), she argued for a connection between bipolar disorder and artistic creativity.[173]
Several films have portrayed characters with traits suggestive of the diagnosis that has been the subject of discussion by psychiatrists and film experts alike. A notable example is Mr. Jones (1993), in which Mr. Jones (Richard Gere) swings from a manic episode into a depressive phase and back again, spending time in a psychiatric hospital and displaying many of the features of the syndrome.[174] In The Mosquito Coast (1986), Allie Fox (Harrison Ford) displays some features including recklessness, grandiosity, increased goal-directed activity and mood lability, as well as some paranoia.[175]
In the progressive metal band Dream Theater song Six Degrees of Inner Turbulence, the lyric of the first movement, About to Crash, describes a girl with bipolar disorder.
Tom Wilkinson portrays a manic-depressive lawyer in Michael Clayton. Matt Damon portrays a manic-depressive whistleblower and FBI informant in The Informant!. In Mark Whitacre, Matt Damon displays bizarre behavior including recklessness and grandiosity.
Next to Normal, a rock musical, concerns a mother who struggles with worsening bipolar disorder and the effect her illness has on her family.
In the Australian TV drama Stingers, Detective Luke Harris (Gary Sweet) is portrayed as having bipolar disorder and shows how his paranoia interfered with his work. As research for the role, Sweet visited a psychiatrist to learn about manic-depressive illness. He said that he left the sessions convinced he had the condition. TV specials, for example the BBC's The Secret Life of the Manic Depressive,[176] MTV's True Life: I'm Bipolar, talk shows, and public radio shows, and the greater willingness of public figures to discuss their own bipolar disorder, have focused on psychiatric conditions, thereby, raising public awareness.
On April 7, 2009, the nighttime drama 90210 on the CW network, aired a special episode where the character Silver was diagnosed with bipolar disorder. A public service announcement (PSA) aired after the episode, directing teens and young adults to the Child and Adolescent Bipolar Foundation website for information and to chat with other teens.[177]
Stacey Slater, a character from the popular BBC soap EastEnders, has been diagnosed with the disorder. After losing her friend Danielle Jones, Stacey began acting strangely; and the character had to come to terms with the prospect that, like her mother, Jean Slater, she suffers from bipolar disorder. The high-profile storyline was developed as part of the BBC's Headroom campaign.[178] The Channel 4 soap Brookside had earlier featured a story about bipolar disorder when the character Jimmy Corkhill was diagnosed with the condition.[179] Dean Sullivan, the actor who played Jimmy, was presented with a Special Achievement Award at the 2003 British Soap Awards for the role.[179]
In Law & Order: Special Victims Unit, Elliot Stabler's daughter, Kathleen Stabler, has been diagnosed with bipolar disorder. It is later revealed that Elliott's mother, Bernadette, also suffered with the disorder; but Bernadette chose not to take medication for it.[citation needed]
In King of the Hill, it is revealed that Kahn, Hank's neighbor, suffers from bipolar disorder. He has severe mood swings when off his medication, being extremely happy and energetic one day and completely depressed to the point of losing all hope of living the next.[citation needed]
References
- ^ Basco, Monica Ramirez, The Bipolar Workbook: Tools for Controlling Your Mood Swings, ISBN 1-59385-162-6, 2006. p.viii
- ^ Lam, D.; Wright, K.; Smith, N. (2004). "Dysfunctional assumptions in bipolar disorder". Journal of Affective Disorders 79 (1-3): 193'199. doi:10.1016/S0165-0327(02)00462-7. PMID 15023494.
- ^ NIMH – What are the symptoms of bipolar disorder?
- ^ Kessler, RC; Chiu, WT; Demler, O; Merikangas, KR; Walters, EE (2005). "Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R)". Arch Gen Psychiat 6 (6): 617'27. doi:10.1001/archpsyc.62.6.617. PMID 15939839. PMC 2847357. http://archpsyc.ama-assn.org/cgi/content/full/62/6/617.
- ^ Frederick K Goodwin and Kay R Jamison.Manic-Depressive Illness Chapter 7, "Epidemiology". Oxford University Press, 1990. ISBN 0-19-503934-3.
- ^ "Bipolar Disorder: Signs and symptoms". Mayo Clinic. http://www.mayoclinic.com/health/bipolar-disorder/DS00356/DSECTION=2.
- ^ NIMH – Bipolar Disorder: NIH Publication 08-3679, Revised 2008
- ^ Mayo Clinic staff. "Bipolar disorder: Tests and diagnosis". MayoClinic.com. http://www.mayoclinic.com/health/bipolar-disorder/DS00356/DSECTION=tests-and-diagnosis. Retrieved 2010-07-19
- ^ "Bipolar Disorder: NIH Publication No. 95-3679". U.S. National Institutes of Health. September 1995. http://web.archive.org/web/20080429204140/http://www.pueblo.gsa.gov/cic_text/health/bipolar/bipolar.htm.
- ^ "Bipolar Disorder: Complications". Mayo Clinic. http://www.mayoclinic.com/health/bipolar-disorder/DS00356/DSECTION=7.
- ^ a b c d Mansell, W. & Pedley, R. The ascent into mania: A review of psychological processes associated with the development of manic symptoms. Clinical Psychology Review, Volume 28, Issue 3, March 2008, Pages 494'520 PMID 17825463
- ^ Robinson LJ, Thompson JM, Gallagher P, Goswami U, Young AH, Ferrier IN, Moore PB. (2006) A meta-analysis of cognitive deficits in euthymic patients with bipolar disorder. J Affect Disord. 2006 July;93(1'3):105'15. PMID 16677713
- ^ Torres IJ, Boudreau VG, Yatham LN. (2007) Neuropsychological functioning in euthymic bipolar disorder: a meta-analysis. Acta Psychiatr Scand Suppl. 2007;(434):17'26. PMID 17688459 (Note: The full text of this study discloses pharmaceutical company funding)
- ^ MacCabe JH, Lambe MP, Cnattingius S, et al. (February 2010). "Excellent school performance at age 16 and risk of adult bipolar disorder: national cohort study". Br J Psychiatry 196 (2): 109'15. doi:10.1192/bjp.bp.108.060368. PMID 20118454.
- ^ Tiihonen J, Haukka J, Henriksson M, et al. (October 2005). "Premorbid intellectual functioning in bipolar disorder and schizophrenia: results from a cohort study of male conscripts". Am J Psychiatry 162 (10): 1904'10. doi:10.1176/appi.ajp.162.10.1904. PMID 16199837.
- ^ "Mad Genius". HowStuffWorks. http://people.howstuffworks.com/mad-genius3.htm. Retrieved September 8, 2008.
- ^ Jamison, K R, Touched with Fire, Free Press, 1993, pp 83 ff.
- ^ Goodwin, F, and Jamison, K R, Manic-Depressive Illness, Oxford University Press, 1990, p 353
- ^ Santosa et al. Enhanced creativity in bipolar disorder patients: A controlled study. J Affect Disord. 2006 November 23; PMID 17126406.
- ^ Rihmer et al. Creativity and mental illness. Psychiatr Hung. 2006;21(4):288'94. PMID 17170470.
- ^ Nowakowska et al. Temperamental commonalities and differences in euthymic mood disorder patients, creative controls, and healthy controls. J Affect Disord. 2005 March;85(1'2):207'15. PMID 15780691.
- ^ Johnson SL (February 2005). "Mania and dysregulation in goal pursuit: a review". Clin Psychol Rev 25 (2): 241'62. doi:10.1016/j.cpr.2004.11.002. PMID 15642648.
- ^ Blairy S, Linotte S, Souery D, et al. (April 2004). "Social adjustment and self-esteem of bipolar patients: a multicentric study". J Affect Disord 79 (1'3): 97'103. doi:10.1016/S0165-0327(02)00347-6. PMID 15023484.
- ^ Kieseppä T, Partonen T, Haukka J, Kaprio J, Lönnqvist J (October 2004). "High concordance of bipolar I disorder in a nationwide sample of twins". Am J Psychiatry 161 (10): 1814'21. doi:10.1176/appi.ajp.161.10.1814. PMID 15465978.
- ^ a b Edvardsen J, Torgersen S, Røysamb E, Lygren S, Skre I, Onstad S, Oien PA. (2008) Heritability of bipolar spectrum disorders. Unity or heterogeneity? J Affect Disord. 2008 March;106(3):229'40. PMID 17692389
- ^ McGuffin, P; Rijsdijk, F; Andrew, M; Sham, P; Katz, R; Cardno, A (2003). "The Heritability of Bipolar Affective Disorder and the Genetic Relationship to Unipolar Depression". Archives of General Psychiatry 60 (5): 497'502. doi:10.1001/archpsyc.60.5.497. PMID 12742871. http://archpsyc.ama-assn.org/cgi/content/abstract/60/5/497.
- ^ Kato, T. (2007). "Molecular genetics of bipolar disorder and depression." Psychiatry Clin Neurosci 61(1): 3'19. PMID 17239033
- ^ Reich, T., P. J. Clayton and G. Winokur (1969). "Family history studies-V The genetics of Mania." American Journal of Psychiatry l25: l358'1369.
- ^ a b Margit Burmeister, Melvin G. McInnis, & Sebastian Zöllner Psychiatric genetics: progress amid controversy Nature Reviews Genetics 9, 527'540 (July 2008) | doi:10.1038/nrg2381
- ^ Barden N., Harvey M., Gagne B., Shink E., Tremblay M., Raymond C., Labbe M., Villeneuve A., Rochette D., Bordeleau L., Stadler H., Holsboer F., and Muller-Myhsok B. (2006). "Analysis of single-nucleotide polymorphisms in genes in the chromosome 12Q24.31 region points to P2RX7 as a susceptibility gene to bipolar affective disorder." Am J Med Genet B Neuropsychiatr Genet.
- ^ Baum, A.E., et al. (2008). A genome-wide association study implicates diacylglycerol kinase eta (DGKH) and several other genes in the etiology of bipolar disorder Molecular Psychiatry, 13(2), 197'207. DOI: 10.1038/sj.mp.4002012
- ^ Burton, P.R., et al. (2007). Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls Nature, 447(7145), 661'678. DOI: 10.1038/nature05911
- ^ Sklar, P., J. W. Smoller, J. Fan, M. A. Ferreira, R. H. Perlis, K. Chambert et al. (2008). Whole-genome association study of bipolar disorder Molecular Psychiatry DOI: 10.1038/sj.mp.4002151
- ^ Ferreira, M., M. O'Donovan, Y. A. Meng, A. Jones I, D. M. Ruderfer1, L. Jones et al. (2008) Collaborative genome-wide association analysis supports a role for ANK3 and CACNA1C in bipolar disorder Nature Genetics 40, 1056'1058
- ^ Segurado R, Detera-Wadleigh SD, Levinson DF, Lewis CM, Gill M, Nurnberger JI Jr, Craddock N, et al. (2003) Genome Scan Meta-Analysis of Schizophrenia and Bipolar Disorder, Part III: Bipolar Disorder. Am J Hum Genet. 73, 49'62. PMID 12802785
- ^ McQuillin, A., N. J. Bass, G. Kalsi, J. Lawrence, V. Puri, K. Choudhury, S. D. Detera-Wadleigh, D. Curtis and H. M. Gurling (2006). "Fine mapping of a susceptibility locus for bipolar and genetically related unipolar affective disorders, to a region containing the C21ORF29 and TRPM2 genes on chromosome 21q22.3." Mol Psychiatry 11(2): 134'142
- ^ Xu, C., F. Macciardi, P. P. Li, I. S. Yoon, R. G. Cooke, B. Hughes, S. V. Parikh, R. S. McIntyre, J. L. Kennedy and J. J. Warsh (2006). "Association of the putative susceptibility gene, transient receptor potential protein melastatin type 2, with bipolar disorder." Am J Med Genet B Neuropsychiatr Genet 141(1): 36'43.
- ^ Barrett TB, Hauger RL, Kennedy JL, Sadovnick AD, Remick RA, Keck PE, McElroy SL, Alexander M, Shaw SH, Kelsoe JR. (May 2003). "Evidence that a single-nucleotide polymorphism in the promoter of the G protein receptor kinase 3 gene is associated with bipolar disorder". Molecular Psychiatry 8 (5): 546'57. doi:10.1038/sj.mp.4001268. PMID 12808434. http://www.nature.com/mp/journal/v8/n5/abs/4001268a.html.
- ^ Zandi PP, Belmonte PL, Willour VL (July 2008). "Association study of Wnt signaling pathway genes in bipolar disorder". Arch. Gen. Psychiatry 65 (7): 785'93. doi:10.1001/archpsyc.65.7.785. PMID 18606951. http://archpsyc.ama-assn.org/cgi/content/full/65/7/785.
- ^ Emma Young (2006). "New gene linked to bipolar disorder". New Scientist. http://www.newscientist.com/article.ns?id=dn8572&feedId=online-news_rss20. Retrieved 2006.
- ^ Frans, E., Sandin, S., Reichenberg, A., Lichtenstein, P., Langstrom, N., Hultman, C. (2008) Advancing Paternal Age and Bipolar Disorder Arch Gen Psychiatry. 2008;65(9):1034'1040.
- ^ a b Serretti A & Mandelli L. (2008) The genetics of bipolar disorder: genome 'hot regions,' genes, new potential candidates and future directions. Mol Psychiatry. 2008 August;13(8):742'71. PMID 18332878
- ^ a b David J. Miklowitz and Kiki D. Chan Prevention of Bipolar Disorder in At-Risk Children: Theoretical Assumptions and Empirical Foundations Dev Psychopathol. Dev Psychopathol. 2008; 20(3): 881'897. doi: 10.1017/S0954579408000424.
- ^ Ross RG (July 2006). "Psychotic and manic-like symptoms during stimulant treatment of attention deficit hyperactivity disorder". Am J Psychiatry 163 (7): 1149'52. doi:10.1176/appi.ajp.163.7.1149. PMID 16816217. http://ajp.psychiatryonline.org/cgi/content/full/163/7/1149.
- ^ DelBello MP, Soutullo CA, Hendricks W, Niemeier RT, McElroy SL, Strakowski SM (April 2001). "Prior stimulant treatment in adolescents with bipolar disorder: association with age at onset". Bipolar Disord 3 (2): 53'7. doi:10.1034/j.1399-5618.2001.030201.x. PMID 11333062. http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=1398-5647&date=2001&volume=3&issue=2&spage=53.
- ^ Soutullo CA, DelBello MP, Ochsner JE (August 2002). "Severity of bipolarity in hospitalized manic adolescents with history of stimulant or antidepressant treatment". J Affect Disord 70 (3): 323'7. doi:10.1016/S0165-0327(01)00336-6. PMID 12128245. http://linkinghub.elsevier.com/retrieve/pii/S0165032701003366.
- ^ Alloy LB, Abramson LY, Urosevic S, Walshaw PD, Nusslock R, Neeren AM. (2005) The psychosocial context of bipolar disorder: environmental, cognitive, and developmental risk factors. Clin Psychol Rev. 2005 December;25(8):1043'75. PMID 16140445
- ^ Gabriele S Leverich a, Robert M Post Course of bipolar illness after history of childhood trauma The Lancet, Volume 367, Issue 9516, Pages 1040'1042, April 1, 2006 doi:10.1016/S0140-6736(06)68450-XCite
- ^ Louisa D. Grandin, Lauren B. Alloy, Lyn Y. Abramson (2007) Childhood Stressful Life Events and Bipolar Spectrum Disorders Journal of Social and Clinical Psychology, 26 (4) pp460'478 doi: 10.1521/jscp.2007.26.4.460
- ^ Strakowski, S.M., DelBello, M.P, Sax, K.W. et al. (1999). "Brain magnetic resonance imaging of structural abnormalities in bipolar disorder," Archives of General Psychiatry, 56:254'60.
- ^ Prefrontal Cortex in Bipolar Disorder Neurotransmitter.net.
- ^ Kempton, M.J., Geddes, J.R, Ettinger, U. et al. (2008). "Meta-analysis, Database, and Meta-regression of 98 Structural Imaging Studies in Bipolar Disorder," Archives of General Psychiatry, 65:1017'1032 see also MRI database at www.bipolardatabase.org.
- ^ Link and reference involving kindling theory
- ^ Brian Koehler, Ph.D., The International Society for the Psychological Treatment Of Schizophrenia and Other Psychoses, Bipolar Disorder, Stress, and the HPA Axis, 2005.
- ^ Stork C, Renshaw PF (July 2005). "Mitochondrial dysfunction in bipolar disorder: evidence from magnetic resonance spectroscopy research". Molecular Psychiatry 10 (2): 900'919. doi:10.1038/sj.mp.4001711. PMID 13594184.
- ^ Malcomb R. Brown; Michael R. Basso (2004). Focus on Bipolar Disorder Research. Nova Science Publishers. pp. 16. ISBN 978-1594540592.
- ^ Lewy AJ, Nurnberger JI, Wehr TA (June 1985). "Supersensitivity to light: possible trait marker for manic-depressive illness". Am J Psychiatry 142 (6): 725'7. PMID 4003592. http://ajp.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=4003592.
- ^ Whalley LJ, Perini T, Shering A, Bennie J (July 1991). "Melatonin response to bright light in recovered, drug-free, bipolar patients". Psychiatry Res 38 (1): 13'9. doi:10.1016/0165-1781(91)90048-T. PMID 1658841.
- ^ Castro LM, Gallant M, Niles LP (December 2005). "Novel targets for valproic acid: up-regulation of melatonin receptors and neurotrophic factors in C6 glioma cells". J. Neurochem. 95 (5): 1227'36. doi:10.1111/j.1471-4159.2005.03457.x. PMID 16313512.
- ^ Hallam KT, Olver JS, Norman TR (July 2005). "Effect of sodium valproate on nocturnal melatonin sensitivity to light in healthy volunteers". Neuropsychopharmacology 30 (7): 1400'4. doi:10.1038/sj.npp.1300739. PMID 15841104.
- ^ Hallam KT, Olver JS, Horgan JE, McGrath C, Norman TR (June 2005). "Low doses of lithium carbonate reduce melatonin light sensitivity in healthy volunteers". Int. J. Neuropsychopharmacol. 8 (2): 255'9. doi:10.1017/S1461145704004894. PMID 15850501.
- ^ Manic-depressive illness FK Goodwin, KR Jamison ' 1990 ' Oxford University Press New York
- ^ Pope HG (1983). "Distinguishing bipolar disorder from schizophrenia in clinical practice: guidelines and case reports". Hospital and Community Psychiatry 34: 322'28.
- ^ Goodwin & Jamison. pp. 108'110.
- ^ Akiskal HS, Yerevanian BI, Davis GC, King D, Lemmi H (February 1985). "The nosologic status of borderline personality: clinical and polysomnographic study". Am J Psychiatry 142 (2): 192'8. PMID 3970243. http://ajp.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=3970243.
- ^ Gunderson JG, Elliott GR (1985). "The interface between borderline personality disorder and affective disorder". Am J Psychiatry 142 (3): 277'288. PMID 2857532.
- ^ McGlashan, TH (1983). "The borderline syndrome:Is it a variant of schizophrenia or affective disorder?". Arch Gen Psychiatry 40 (12): 1319'1323. PMID 6651467.
- ^ Pope HG Jr, Jonas JM, Hudson JI, Cohen BM, Gunderson JG (1983). "The validity of DSM-III borderline personality disorder: A phenomenologic, family history, treatment response, and long term follow up study". Arch Gen Psychiatry 40 (1): 23'30. PMID 6849616.
- ^ Psychiatric Times. Clinically Useful Psychiatric Scales: Bipolar Spectrum Diagnostic Scale. Retrieved March 9, 2009.
- ^ Ghaemi N. Sensitivity and specificity of a new bipolar spectrum diagnostic scale. J Affect Disord. 2005;84:273'277.
- ^ Akiskal HS, Benazzi F (May 2006). "The DSM-IV and ICD-10 categories of recurrent [major] depressive and bipolar II disorders: evidence that they lie on a dimensional spectrum". J Affect Disord. 92 (1): 45'54. doi:10.1016/j.jad.2005.12.035. PMID 16488021.
- ^ American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th, text revision (DSM-IV-TR) ed. 2000. ISBN 0-89042-025-4. Bipolar Disorder.
- ^ DSM-IV-TR. Bipolar I Disorder.
- ^ DSM-IV-TR. Diagnostic criteria for 296.89 Bipolar II Disorder.
- ^ DSM-IV-TR. Diagnostic criteria for 301.13 Cyclothimic Disorder.
- ^ DSM-IV-TR. Not Otherwise Specified (NOS).
- ^ DSM-IV-TR. Longitudinal course specifiers for mood disorders.
- ^ Kessler, RC; McGonagle, KA; Zhao, S; Nelson, CB; Hughes, M; Eshleman, S; Wittchen, HU; Kendler, KS (1994). "Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States". Archives of General Psychiatry 51 (1): 8'19. doi:10.1001/archpsyc.51.1.8 (inactive 2008-06-25). PMID 8279933. http://archpsyc.ama-assn.org/cgi/content/abstract/51/1/8.
- ^ Angst, J; Selloro, R (September 15, 2000). "Historical perspectives and natural history of bipolar disorder". Biological Psychiatry 48 (6): 445'457. doi:10.1016/S0006-3223(00)00909-4. PMID 11018218.
- ^ Mackin, P; Young, AH (2004). "Rapid cycling bipolar disorder: historical overview and focus on emerging treatments". Bipolar Disorders 6 (6): 523'529. doi:10.1111/j.1399-5618.2004.00156.x. PMID 15541068.
- ^ Papolos, DF; Veit, S; Faedda, GL; Saito, T; Lachman, HM (1998). "Ultra-ultra rapid cycling bipolar disorder is associated with the low activity catecholamine-O-methyltransferase allele". Molecular Psychiatry 3 (4): 346'349. doi:10.1038/sj.mp.4000410. PMID 9702745. http://www.nature.com/mp/journal/v3/n4/abs/4000410a.html.
- ^ S. Nassir Ghaemi (2001). "Bipolar Disorder: How long does it usually take for someone to be diagnosed for bipolar disorder?". Archived from the original on December 7, 2006. http://web.archive.org/web/20061207224847/http://www.familyaware.org/expertprofiles/drghaemi4.asp. Retrieved February 20, 2007.
- ^ Roy H. Perlis (2005). "Misdiagnosis of Bipolar Disorder". American Journal of Managed Care. http://www.ajmc.com/Article.cfm?Menu=1&ID=2969. Retrieved February 20, 2007.
- ^ Hypomanic Check List Questionnaire (HCL-32)
- ^ Amy K. Cuellar, Sheri L. Johnson and Ray Winters (2005) Distinctions between bipolar and unipolar depression Clinical Psychology Review, Vol 25, 3, May, P 307-339 PMID 15792852 doi = 10.1016/j.cpr.2004.12.002
- ^ Benazzi F. (2007) Is there a continuity between bipolar and depressive disorders? Psychother Psychosom 76(2):70-6. PMID 17230047
- ^ Depression and Bipolar Support Alliance: About Mood Disorders
- ^ Goodwin & Jamison, 1990.
- ^ Sagman D and Tohen M (2009). "Comorbidity in Bipolar Disorder: The Complexity of Diagnosis and Treatment". Psychiatric Times. http://www.psychiatrictimes.com/display/article/10168/1391541.
- ^ Kranowitz, C.S. & Post, R., (1996). Ultra-rapid and ultradian cycling in bipolar affective illness. British Journal of Psychiatry, 168, 314'323.
- ^ Naomi A. Schapiro Bipolar Disorders in Children and Adolescents J Pediatr Health Care. 2005;19(3):131'141.
- ^ Bipolar labels for children stir concern ' The Boston Globe
- ^ Trinh NH, Forester B (2007). "Bipolar Disorder in the Elderly: Differential Diagnosis and Treatment". Psychiatric Times 24 (14). http://www.psychiatrictimes.com/bipolar-disorder/article/10168/54481.
- ^ Becker T, Kilian R. (2006) Psychiatric services for people with severe mental illness across western Europe: what can be generalized from current knowledge about differences in provision, costs and outcomes of mental health care? Acta Psychiatrica Scandinavica Supplement, 429, 9'16. PMID 16445476
- ^ McGurk, SR, Mueser KT, Feldman K, Wolfe R, Pascaris A (2007). Cognitive training for supported employment: 2'3 year outcomes of a randomized controlled trial. Am J Psychiatry. March;164(3):437'41. PMID 17329468
- ^ (Lam et al., 1999; Johnson & Leahy, 2004; Basco & Rush, 2005; Miklowitz & Goldstein, 1997; Frank, 2005.
- ^ Zaretsky AE, Rizvi S, & Parikh SV. (2007). How well do psychosocial interventions work in bipolar disorder? Can J Psychiatry, January;52(1):14'21.
- ^ Havens LL, Ghaemi SN. (2005) Existential despair and bipolar disorder: the therapeutic alliance as a mood stabilizer. Am J Psychother. 59(2):137'47 PMID 16170918
- ^ Geddes JR, Burgess S, Hawton K, Jamison K, Goodwin GM (February 2004). "Long-term lithium therapy for bipolar disorder: systematic review and meta-analysis of randomized controlled trials". Am J Psychiatry 161 (2): 217'22. doi:10.1176/appi.ajp.161.2.217. PMID 14754766.
- ^ Bauer MS, Mitchner L (January 2004). "What is a "mood stabilizer"? An evidence-based response". Am J Psychiatry 161 (1): 3'18. doi:10.1176/appi.ajp.161.1.3. PMID 14702242.
- ^ Poolsup N, Li Wan Po A, de Oliveira IR. (2000) Systematic overview of lithium treatment in acute mania. J Clin Pharm Ther 25: 139'156 PMID: 10849192
- ^ Macritchie K, Geddes JR, Scott J, Haslam D, de Lima M, Goodwin G. (2002). (abstract) "Valproate for acute mood episodes in bipolar disorder". The Cochrane Database of Systematic Reviews (John Wiley and Sons, Ltd.) (2): CD004052. doi:10.1002/14651858.CD004052. ISSN 1464-780X. PMID 12535506. http://www.cochrane.org/reviews/en/ab004052.html (abstract).
- ^ Calabrese JR, Bowden CL, Sachs GS, Ascher JA, Monaghan E, Rudd GD (February 1999). "A double-blind placebo-controlled study of lamotrigine monotherapy in outpatients with bipolar I depression. Lamictal 602 Study Group". J Clin Psychiatry 60 (2): 79'88. PMID 10084633.
- ^ Now Approved: ZYPREXA for maintenance therapy for bipolar disorder.[dead link] Official Zyprexa Website.
- ^ Tohen M, Greil W, Calabrese JR (July 2005). "Olanzapine versus lithium in the maintenance treatment of bipolar disorder: a 12-month, randomized, double-blind, controlled clinical trial". Am J Psychiatry 162 (7): 1281'90. doi:10.1176/appi.ajp.162.7.1281. PMID 15994710.
- ^ "Treatment of refractory and rapid-cycling bipolar disorder". http://www.wpic.pitt.edu/stanley/1stbipconf/bipolar2.htm#trtref.
- ^ Sachs, GS, MD, et al. (2007) Effectiveness of Adjunctive Antidepressant Treatment for Bipolar Depression New England Journal of Medicine, Volume 356:1711'1722 (Abstract).
- ^ Bipolar surprise: mood disorder endures antidepressant setback. Science News, March 31, 2007, vol. 171, #13, p.196
- ^ Results for Triacetyluridine tau decreases depressive symptoms and increases brain ph in bipolar patients
- ^ Omega 3 Fatty Acids in Bipolar Disorder A Preliminary Double-blind, Placebo-Controlled Trial | Treatments
- ^ Bergen M (1999). Riding the Roller Coaster: Living with Mood Disorders. Wood Lake Publishing Inc.. ISBN 9781896836317. http://books.google.com/?id=s4dVLeND9l0C&lpg=PP1&dq=riding%20the%20roller%20coaster%2C%20living%20with%20mood&pg=PA26#v=onepage&q=.
- ^ "Introduction". cs.umd.edu. http://www.cs.umd.edu/class/spring2004/cmsc434/teams/rise/Introduction.htm. Retrieved February 16, 2008.
- ^ Judd Lewis L.; Aksikal Hagop S.; Schettler Pamela J. ; Endicott Jean; Leon Andrew C.; Solomon David A.; Coryell William; Maser Jack D.; Keller Martin B. (2005) Psychosocial disability in the course of bipolar I and II disorders : A prospective, comparative, longitudinal study Archives of General Psychiatry, vol. 62, no12, pp. 1322'1330
- ^ Ösby, U; Brandt, L; Correia, N; Ekbom, A; Sparén, P (2001). "Excess Mortality in Bipolar and Unipolar Disorder in Sweden". Archives of General Psychiatry 58 (9): 844'850. doi:10.1001/archpsyc.58.9.844. PMID 11545667. http://archpsyc.ama-assn.org/cgi/content/abstract/58/9/844.
- ^ Tohen M, Zarate CA Jr, Hennen J, Khalsa HM, Strakowski SM, Gebre-Medhin P, Salvatore P, Baldessarini RJ. (2003) The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence Am J Psychiatry. 2003 December;160(12):2099-107.
- ^ Basco, Monica Ramirez, The Bipolar Workbook: Tools for Controlling Your Mood Swings, ISBN 1-59385-162-6, 2006. p2
- ^ Bipolar Disorder webpage from ADAM Illustrated Health Encyclopedia at About.com
- ^ Perry A, Tarrier N, Morriss R, McCarthy E, Limb K (January 1999). "Randomised controlled trial of efficacy of teaching patients with bipolar disorder to identify early symptoms of relapse and obtain treatment". BMJ 318 (7177): 149'53. PMID 9888904. PMC 27688. http://bmj.com/cgi/pmidlookup?view=long&pmid=9888904.
- ^ Kelly, M., Bipolar and the Art of Roller-coaster Riding, Two Trees Media 2000, 2005
- ^ Roger S. McIntyre, MD, Joanna K. Soczynska, and Jakub Konarski. "Bipolar Disorder: Defining Remission and Selecting Treatment". Psychiatric Times, October 2006, Vol. XXIII, No. 11. http://www.psychiatrictimes.com/article/showArticle.jhtml?articleId=193400986.
- ^ Leslie Citrome, MD, MPH; Joseph F. Goldberg, MD. "Bipolar disorder is a potentially fatal disease". http://www.postgradmed.com/issues/2005/02_05/comm_citrome.htm.[dead link]
- ^ Psychopathologic Correlates of Suicidal Ideation in Major Depressive Outpatients: Is It All Due to Unrecognized (Bipolar) Depressive Mixed States?
- ^ Soldani, Federico; Sullivan, PF; Pedersen, NL (April 2005). "Mania in the Swedish Twin Registry: criterion validity and prevalence". Australian and New Zealand of Psychiatry 39 (4): 235'43. doi:10.1111/j.1440-1614.2005.01559.x. PMID 15777359.
- ^ Judd, Lewis L.; Akiskal, HS (January 2003). "The prevalence and disability of bipolar spectrum disorders in the US population: re-analysis of the ECA database taking into account subthreshold cases". Journal of Affective Disorders 73 (1'2): 123'31. doi:10.1016/S0165-0327(02)00332-4. PMID 12507745. http://linkinghub.elsevier.com/retrieve/pii/S0165032702003324.
- ^ Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC. (2007) Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication Arch Gen Psychiatry. May;64(5):543'52.
- ^ Phelps, J. (2006) Bipolar Disorder: Particle or Wave? DSM Categories or Spectrum Dimensions? Psychiatric Times
- ^ Christie KA, Burke JD Jr, Regier DA, Rae DS, Boyd JH, Locke BZ (1988). (abstract) "Epidemiologic evidence for early onset of mental disorders and higher risk of drug abuse in young adults". Am J Psychiatry 145 (8): 971'975. PMID 3394882. http://www.ajp.psychiatryonline.org/cgi/content/abstract/145/8/971 (abstract). Retrieved July 1, 2007.[dead link]
- ^ Goodwin & Jamison. p. 121.
- ^ American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders: Fourth Edition Text Revision (DSM-IV-TR). 1'943
- ^ World Health Organization (1979) International classification of diseases. 9th ed.
- ^ Kraepelin (1921) Manic-Depressive Insanity and Paranoia.
- ^ Loranger and Levine (1978) Age at onset of bipolar affective illness. Archives of General Psychiatry. 35 1345'1348
- ^ Goodwin and Redfield Jamison (1990) Childhood and Adolescence. Manic-Depressive Illness. 186'209
- ^ Anthony and Scott (1960) Manic-depressive psychosis in childhood. Journal of Child Psychology and Psychiatry. 1 53'72
- ^ Hudziak, Althoff, Rettew, Derks and Faraone (2005) The prevalence and genetic architecture of CBCL-juvenile bipolar disorder. Biological Psychiatry. 58 562'8
- ^ Lewinsohn, Klein and Seeley (1995) Bipolar disorders in a community sample of older adolescents: Prevalence, phenomenology, comorbidity, and course. Journal of the American Academy of Child and Adolescent Psychiatry. 34 454'463
- ^ Weller, Weller, Tucker and Fristad (1986) Mania in prepubertal children: Has it been underdiagnosed? Journal of Affective Disorders. 11 151'154
- ^ a b c Wozniak, Biederman, Kiely, Ablon, Faraone, Mundy and Mennin (1995) Mania-like symptoms suggestive of childhood onset bipolar disorder in clinically referred children. Journal of the American Academy of Child and Adolescent Psychiatry. 34 867'876
- ^ a b c Wozniak, Biederman, Mundy, Mennin and Faraone (1995) A pilot family study of childhood-onset mania. Journal of the American Academy of Child and Adolescent Psychiatry. 34 1577'1583
- ^ Carlson, Bromet, Driessens, Mojtabai and Schwartz (2002) Age at onset, childhood psychopathology, and two-year outcome in psychotic bipolar disorder. Am J Psychiatry. 159 307'9.
- ^ Meyer, Carlson, Wiggs, Martinez, Ronsaville, Klimes-Dougan, Gold and Radke-Yarrow (2004) A prospective study of the association among impaired executive functioning, childhood attentional problems, and the development of bipolar disorder. Dev Psychopathol. 16 461'76
- ^ Biederman (2003) Pediatric bipolar disorder coming of age. Biological Psychiatry. 53 931'934
- ^ Biederman, Mick, Faraone, Spencer, Wilens and Wozniak (2003) Current concepts in the validity, diagnosis and treatment of paedatric bipolar disorder. International Journal of Neuropsychopharmacology. 6 293'300
- ^ Geller and Luby (1997) Child and adolescent bipolar disorder: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 36 1168'1176
- ^ Geller and Tillman (2005) Prepubertal and early adolescent bipolar I disorder: review of diagnostic validation by Robins and Guze criteria. Journal of Clinical Psychiatry. 66 Suppl 7 21'28
- ^ (2007) Practice Parameter for the Assessment and Treatment of Children and Adolescents With Bipolar Disorder. J Am Acad Child Adolesc Psychiatry. 46 107'125
- ^ Moreno C, Laje G, Blanco C, Jiang H, Schmidt AB, Olfson M. (September 2007) "National trends in the outpatient diagnosis and treatment of bipolar disorder in youth," Archives of General Psychiatry. 64(9):1032'9. PMID 17768268
- ^ National Institute of Health and Clinical Excellence (2006). National clinical practice guidelines number 38: Bipolar disorder: the management of bipolar disorder in adults, children and adolescents in primary and secondary care. London: National Collaborating Centre for Mental Health.
- ^ Meyer TD, Koßmann-Böhm S, Schlottke PF. Do child psychiatrists in Germany diagnose bipolar disorders in children and adolescents? Result from a survey. Bipolar Disorders, 2004; 6: 426 ' 431
- ^ Parry P, Furber G, Allison S. The paediatric bipolar hypothesis: the view from Australia and New Zealand. Child and Adolescent Mental Health. (in press)
- ^ Carlson G, Meyer S. Phenomenology and diagnosis of bipolar disorder in children, adolescents, and adults: Complexities and developmental issues Development and Psychopathology 2006; 18:939'969
- ^ Harris J. Child & adolescent psychiatry: the increased diagnosis of 'juvenile bipolar disorder': what are we treating? Psychiatr Serv 2005; 56: 529 ' 531
- ^ McClellan J. Commentary: treatment guidelines for child and adolescent bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry 2005; 44: 236'239
- ^ Laurel Williams. Mental health and children: Too often the system conspires to treat behavioural problems with pills. Los Angeles Times Dec 14, 2008 available at: http://www.latimes.com/news/opinion/commentary/la-oe-williams14-2008dec14,0,3774809.story
- ^ Bipolar Children: Cutting-edge controversy, insights and research. Childhood in America series. editor Sharna Olfman. 2007. Praeger press. Westport CT. http://www.amazon.com/Bipolar-Children-Cutting-Edge-Controversy-Childhood/dp/0275997308/ref=sr_1_11?ie=UTF8&s=books&qid=1245833103&sr=8-11
- ^ USATODAY.com ' New antipsychotic drugs carry risks for children
- ^ Glahn, Bearden, Caetano, Fonseca, Najt, Hunter, Pliszka, Olvera and Soares (2005) Declarative memory impairment in pediatric bipolar disorder. Bipolar Disord. 7 546'54
- ^ McClure, Treland, Snow, Dickstein, Towbin, Charney, Pine and Leibenluft (2005) Memory and learning in pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 44 461'9
- ^ Pavuluri, Schenkel, Aryal, Harral, Hill, Herbener and Sweeney (2006) Neurocognitive function in unmedicated manic and medicated euthymic pediatric bipolar patients. Am J Psychiatry. 163 286'93
- ^ Biederman, Kwon, Wozniak, Mick, Markowitz, Fazio and Faraone (2004) Absence of gender differences in pediatric bipolar disorder: Findings from a large sample of referred youth. Journal of Affective Disorders. 83 207'214
- ^ a b Caetano, Olvera, Hunter, Hatch, Najt, Bowden, Pliszka and Soares (2006) Association of psychosis with suicidality in pediatric bipolar I, II and bipolar NOS patients. J Affect Disord. 91 33'7
- ^ a b Wozniak, Biederman, Kiely, Ablon and Faraone (1993) Prepubertal mania revisited. Scientific Proceedings of the Annual Meeting of the American Academy of Child and Adolescent Psychiatry
- ^ Bipolar Phases in Children[dead link]
- ^ Goldstein, Birmaher, Axelson, Ryan, Strober, Gill, Valeri, Chiappetta, Leonard, Hunt, Bridge, Brent and Keller (2005) History of suicide attempts in pediatric bipolar disorder: factors associated with increased risk. Bipolar Disord. 7 525'35
- ^ Depp CA, Jeste DV. (2004) Bipolar disorder in older adults: a critical review Bipolar Disord. 2004 October;6(5):343'67.
- ^ Liddell, Henry George and Robert Scott (1980). A Greek-English Lexicon (Abridged Edition). United Kingdom: Oxford University Press. ISBN 0-19-910207-4.
- ^ "Circular insanity, 150 years on". http://www.ncbi.nlm.nih.gov/pubmed/15506718. Retrieved 2008-04-12.
- ^ Millon, Theordore (1996). Disorders of Personality: DSM-IV-TM and Beyond. New York: John Wiley and Sons. pp. 290. ISBN 0-471-01186-X.
- ^ Kraepelin, Emil (1921) Manic-depressive Insanity and Paranoia ISBN 0-405-07441-7
- ^ Goodwin & Jamison. pp. 60'61.
- ^ Goodwin & Jamison. p62
- ^ Jamison, Kay Redfield (1995). An Unquiet Mind: A Memoir of Moods and Madness. New York: Knopf.. ISBN 0-330-34651-2.
- ^ Jamison, Kay Redfield (1996). Touched With Fire: Manic-Depressive Illness and the Artistic Temperament. New York: The Free Press: Macmillian, Inc.. ISBN 0-684-83183-X.
- ^ Robinson DJ (2003). Reel Psychiatry:Movie Portrayals of Psychiatric Conditions. Port Huron, Michigan: Rapid Psychler Press. pp. 78'81. ISBN 1-894328-07-8.
- ^ Robinson (Reel Psychiatry:Movie Portrayals of Psychiatric Conditions), p. 84'85
- ^ "The Secret Life of the Manic Depressive". BBC. 2006. http://www.bbc.co.uk/health/tv_and_radio/secretlife_index.shtml. Retrieved February 20, 2007.
- ^ "Child and Adolescent Bipolar Foundation special 90210 website". CABF. 2009. http://www.bpkids.org/90210. Retrieved April 7, 2009.
- ^ "EastEnders' Stacey faces bipolar disorder". BBC Press Office. May 14, 2009. http://www.bbc.co.uk/pressoffice/pressreleases/stories/2009/05_may/14/stacey.shtml. Retrieved May 28, 2009.
- ^ a b Tinniswood, Rachael (May 14, 2003). "The Brookie boys who shone at soap awards show". Liverpool Echo (Mirror Group Newspapers).
Cited texts
- Goodwin FK, Jamison KR (1990). Manic-Depressive Illness. New York: Oxford University Press. ISBN 0-19-503934-3.
- Goodwin FK, Jamison KR (2007). Manic-Depressive Illness: Bipolar Disorders and Recurrent Depression, 2nd Edition. New York: Oxford University Press. ISBN 0-19-513579-2.
Further reading
- Contemporary first-person accounts
- Simon, Lizzie. 2002. Detour: My Bipolar Road Trip in 4-D. New York: Simon and Schuster. ISBN 0-7434-4659-3.
- Behrman, Andy. 2002. Electroboy: A Memoir of Mania. New York: Random House, 2002. ISBN 0-375-50358-7.
- Lovelace, David. 2008. Scattershot: My Bipolar Family. New York: Dutton Adult, 2008. ISBN 0-525-95078-8.
- Managing bipolar disorder
- Berk, Lesley (March 5, 2009). Living with Bipolar. Vermilion. ISBN 9780091924256.
- Bipolar disorder in children
- Raeburn, Paul. 2004. Acquainted with the Night: A Parent's Quest to Understand Depression and Bipolar Disorder in His Children.
- Earley, Pete. Crazy. 2006. New York: G. P. Putnam's Sons. ISBN 0-399-15313-6. A father's account of his son's bipolar disorder.
- Classic works on bipolar disorder
- Kraepelin, Emil. 1921. Manic-depressive Insanity and Paranoia ISBN 0-405-07441-7 (English translation of the original German from the earlier eighth edition of Kraepelin's textbook ' now outdated, but a work of major historical importance).
- Mind Over Mood: Cognitive Treatment Therapy Manual for Clients by Christine Padesky, Dennis Greenberger. ISBN 0-89862-128-3
External links
- Bipolar Disorder overview from the U.S. National Institute of Mental Health website
- NICE Bipolar Disorder clinical guidelines from the U.K. National Institute for Health and Clinical Excellence website
- Bipolar Disorder at the Open Directory Project
|
||||||||||||||||||||||||||||||
|
SOURCES.COM is an online portal and directory for journalists, news media, researchers and anyone seeking experts, spokespersons, and reliable information resources. Use SOURCES.COM to find experts, media contacts, news releases, background information, scientists, officials, speakers, newsmakers, spokespeople, talk show guests, story ideas, research studies, databases, universities, associations and NGOs, businesses, government spokespeople. Indexing and search applications by Ulli Diemer and Chris DeFreitas.
For information about being included in SOURCES as a expert or spokesperson see the FAQ . For partnerships, content and applications, and domain name opportunities contact us.