
| Home | Sources Directory | News Releases | Calendar | Articles | | Contact | |
Public health
Public health is "the science and art of preventing disease, prolonging life and promoting health through the organized efforts and informed choices of society, organizations, public and private, communities and individuals." (1920, C.E.A. Winslow)[1] It is concerned with threats to the overall health of a community based on population health analysis. The population in question can be as small as a handful of people or as large as all the inhabitants of several continents (for instance, in the case of a pandemic). Public health is typically divided into epidemiology, biostatistics and health services. Environmental, social, behavioral, and occupational health are other important subfields.
There are 2 distinct characteristics of public health:
1. It deals with preventive rather than curative aspects of health
2. It deals with population-level, rather than individual-level health issues
The focus of public health intervention is to prevent rather than treat a disease through surveillance of cases and the promotion of healthy behaviors. In addition to these activities, in many cases treating a disease may be vital to preventing it in others, such as during an outbreak of an infectious disease. Hand washing, vaccination programs and distribution of condoms are examples of public health measures.
The goal of public health is to improve lives through the prevention and treatment of disease. The United Nations' World Health Organization defines health as "a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity."[2]
Contents |
[edit] Objectives
The focus of a public health intervention is to prevent rather than treat a disease through surveillance of cases and the promotion of healthy behaviors. In addition to these activities, in many cases treating a disease can be vital to preventing its spread to others, such as during an outbreak of infectious disease or contamination of food or water supplies. Vaccination programs and distribution of condoms are examples of public health measures.
Most countries have their own government public health agencies, sometimes known as ministries of health, to respond to domestic health issues. In the United States, the front line of public health initiatives are state and local health departments. The United States Public Health Service (PHS), led by the Surgeon General of the United States, and the Centers for Disease Control and Prevention, headquartered in Atlanta, are involved with several international health activities, in addition to their national duties.
There is a vast discrepancy in access to health care and public health initiatives between developed nations and developing nations. In the developing world, public health infrastructures are still forming. There may not be enough trained health workers or monetary resources to provide even a basic level of medical care and disease prevention. As a result, a large majority of disease and mortality in the developing world results from and contributes to extreme poverty. For example, many African governments spend less than USD$10 per person per year on health care, while, in the United States, the federal government spent approximately USD$4,500 per capita in 2000.
Many diseases are preventable through simple, non-medical methods. For example, research has shown that the simple act of hand washing can prevent many contagious diseases.[3]
Public health plays an important role in disease prevention efforts in both the developing world and in developed countries, through local health systems and through international non-governmental organizations.
The two major postgraduate professional degrees related to this field are the Master of Public Health (MPH) or the (much rarer) Doctor of Public Health (DrPH). Many public health researchers hold PhDs in their fields of speciality, while some public health programs confer the equivalent Doctor of Science degree instead.
[edit] History of public health
In some ways, public health is a modern concept, although it has roots in antiquity. From the beginnings of human civilization, it was recognized that polluted water and lack of proper waste disposal spread communicable diseases (theory of miasma). Early religions attempted to regulate behavior that specifically related to health, from types of food eaten, to regulating certain indulgent behaviors, such as drinking alcohol or sexual relations. The establishment of governments placed responsibility on leaders to develop public health policies and programs in order to gain some understanding of the causes of disease and thus ensure social stability prosperity, and maintain order.
The term "healthy city" used by today's public health advocates reflects this ongoing challenge to collective physical well-being that results from crowded conditions and urbanization.
[edit] Early public health interventions
By Roman times, it was well understood that proper diversion of human waste was a necessary tenet of public health in urban areas. The Chinese developed the practice of variolation following a smallpox epidemic around 1000 BC. An individual without the disease could gain some measure of immunity against it by inhaling the dried crusts that formed around lesions of infected individuals. Also, children were protected by inoculating a scratch on their forearms with the pus from a lesion. This practice was not documented in the West until the early-1700s, and was used on a very limited basis. The practice of vaccination did not become prevalent until the 1820s, following the work of Edward Jenner to treat smallpox.
During the 14th century Black Death in Europe, it was believed that removing bodies of the dead would further prevent the spread of the bacterial infection. This did little to stem the plague, however, which was most likely spread by rodent-borne fleas. Burning parts of cities resulted in much greater benefit, since it destroyed the rodent infestations. The development of quarantine in the medieval period helped mitigate the effects of other infectious diseases. However, according to Michel Foucault, the plague model of governmentality was later controverted by the cholera model. A Cholera pandemic devastated Europe between 1829 and 1851, and was first fought by the use of what Foucault called "social medicine", which focused on flux, circulation of air, location of cemeteries, etc. All those concerns, born of the miasma theory of disease, were mixed with urbanistic concerns for the management of populations, which Foucault designated as the concept of "biopower". The German conceptualized this in the Polizeiwissenschaft ("Science of police").
The science of epidemiology was founded by John Snow's identification of a polluted public water well as the source of an 1854 cholera outbreak in London. Dr. Snow believed in the germ theory of disease as opposed to the prevailing miasma theory. Although miasma theory correctly teaches that disease is a result of poor sanitation, it was based upon the prevailing theory of spontaneous generation. Germ theory developed slowly: despite Anton van Leeuwenhoek's observations of Microorganisms, (which are now known to cause many of the most common infectious diseases) in the year 1680, the modern era of public health did not begin until the 1880s, with Louis Pasteur's germ theory and production of artificial vaccines.
Other public health interventions include latrinization, the building of sewers, the regular collection of garbage followed by incineration or disposal in a landfill, providing clean water and draining standing water to prevent the breeding of mosquitos. This contribution was made by Edwin Chadwick in 1843 who published a report on the sanitation of the working class population in Great Britain at the time. So began the inception of the modern public health. The industrial revolution had initially caused the spread of disease through large conurbations around workhouses and factories. These settlements were cramped and primitive and there was no organised sanitation. Disease was innevitable and its incubation in these areas was encouraged by the poor lifestyle of the inhabitants....
[edit] Modern public health
As the prevalence of infectious diseases in the developed world decreased through the 20th century, public health began to put more focus on chronic diseases such as cancer and heart disease. An emphasis on physical exercise was reintroduced.[citation needed]
In America, public health worker Dr. Sara Josephine Baker lowered the infant mortality rate using preventative methods. She established many programs to help the poor in New York City keep their infants healthy. Dr. Baker led teams of nurses into the crowded neighborhoods of Hell's Kitchen and taught mothers how to dress, feed, and bathe their babies. After World War I many states and countries followed her example in order to lower infant mortality rates.[citation needed]
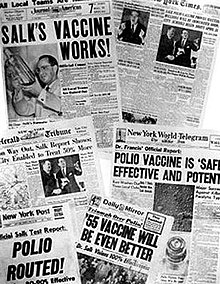
During the 20th century, the dramatic increase in average life span is widely credited to public health achievements, such as vaccination programs and control of infectious diseases, effective safety policies such as motor-vehicle and occupational safety, improved family planning, chlorination of drinking water, smoke-free measures, and programs designed to decrease chronic disease.
Meanwhile, the developing world remained plagued by largely preventable infectious diseases, exacerbated by malnutrition and poverty. Front-page headlines continue to present society with public health issues on a daily basis: emerging infectious diseases such as SARS, making its way from China (see Public health in China) to Canada and the United States; prescription drug benefits under public programs such as Medicare; the increase of HIV-AIDS among young heterosexual women and its spread in South Africa; the increase of childhood obesity and the concomitant increase in type II diabetes among children; the impact of adolescent pregnancy; and the ongoing social, economic and health disasters related to the 2004 Tsunami and Hurricane Katrina in 2005.[citation needed] These are all ongoing public health challenges.
Since the 1980s, the growing field of population health has broadened the focus of public health from individual behaviors and risk factors to population-level issues such as inequality, poverty, and education. Modern public health is often concerned with addressing determinants of health across a population, rather than advocating for individual behaviour change. There is a recognition that our health is affected by many factors including where we live, genetics, our income, our educational status and our social relationships - these are known as "social determinants of health." A social gradient in health runs through society, with those that are poorest generally suffering the worst health. However even those in the middle classes will generally have worse health outcomes than those of a higher social stratum.[4] The new public health seeks to address these health inequalities by advocating for population-based policies that improve health in an equitable manner.
[edit] Schools of public health
In the US, the Welch-Rose Report of 1915 has been viewed as the basis for the critical movement in the history of the institutional schism between public health and medicine because it led to the establishment of schools of public health supported by the Rockefeller Foundation.[5][6] The report was authored by William Welch, founding dean of the Johns Hopkins Bloomberg School of Public Health, and Wycliffe Rose of the Rockfeller Foundation. The report focused more on research than practical education.[5][7] Some have blamed the Rockfeller Foundation's 1916 decision to support the establishment of schools of public health for creating the schism between public health and medicine and legitimizing the rift between medicine's laboratory investigation of the mechanisms of disease and public health's nonclinical concern with environmental and social influences on health and wellness.[5][8]
Even though schools of public health had already been established in Europe and North Africa, the US had still maintained the traditional system of housing faculties of public health within their medical institutions. However, a year following the Welch-Rose report, the Johns Hopkins School of Hygiene and Public Health was founded in 1916. By 1922, schools of public health were established in Columbia, Harvard and Yale universities. By 1999 there were twenty nine schools of public health in the US, enrolling around fifteen thousand students.[5][9]
Over the years, the types of students and training provided have also changed. In the beginning, students who enrolled in public health schools had already obtained a medical degree. However, in 1978, 69% of students enrolled in public health schools had only a bachelors degree. Public health school training had evolved from a second degree for medical professionals to a primary public health degree with a focus on the six core disciplines of biostatistics, epidemiology, health services administration, health education, behavioral science and environmental science.[5][9]
[edit] Education and training
Schools of public health offer a variety of degrees which generally fall into two categories: professional or academic.[10]
Professional degrees are oriented towards practice in public health settings. The Master of Public Health (M.P.H.), Doctor of Public Health (Dr.PH.) and the Master of Health Care Administration (M.H.A.) are examples of degrees which are geared towards people who want careers as practitioners of public health in health departments, managed care and community-based organizations, hospitals and consulting firms among others. Master of Public Health (M.P.H.) degrees broadly fall into two categories, those that put more emphasis on an understanding of epidemiology and statistics as the scientific basis of public health practice and those that include a more eclectic range of methodologies. A Master of Science of Public Health (M.S.P.H.) is granted to students who do extra studies in research, and often have had little health background before entering the degree.
Academic degrees are more oriented towards those with interests in the scientific basis of public health and preventive medicine who wish to pursue careers in research, university teaching in graduate programs, policy analysis and development, and other high-level public health positions. Examples of academic degrees are the Master of Science (M.S.), Doctor of Philosophy (Ph.D.), and Doctor of Science (Sc.D.). The doctoral programs are distinct from the M.P.H. and other professional programs by the addition of advanced coursework and the nature and scope of a dissertation research project.
The Association of Schools of Public Health[11] represents Council on Education for Public Health (CEPH) accredited schools of public health in the United States, Puerto Rico, and Mexico.[12]
Delta Omega is the honorary society for graduate studies in public health. The society was founded in 1924 at the Johns Hopkins School of Hygiene and Public Health. Currently, there are approximately 50 chapters throughout the United States and Puerto Rico.[13]
[edit] Public health programs
Today, most governments recognize the importance of public health programs in reducing the incidence of disease, disability, and the effects of aging, although public health generally receives significantly less government funding compared with medicine. In recent years, public health programs providing vaccinations have made incredible strides in promoting health, including the eradication of smallpox, a disease that plagued humanity for thousands of years.
An important public health issue facing the world currently is HIV/AIDS.[14] Antibiotic resistance is another major concern, leading to the reemergence of diseases such as Tuberculosis.
Another major public health concern is diabetes[15]. In 2006, according to the World Health Organization, at least 171 million people worldwide suffered from diabetes. Its incidence is increasing rapidly, and it is estimated that by the year 2030, this number will double. However, in a June 2010 editorial in the medical journal The Lancet, the authors opined that "The fact that type 2 diabetes, a largely preventable disorder, has reached epidemic proportion is a public health humiliation."[16] (Type 1 diabetes mellitus is not preventable, however.)
A controversial aspect of public health is the control of smoking.[17] Non-communicable diseases caused by smoking have been threatening public health because it requires a long term strategy for improving unlike the communicable diseases which take a shorter period to be improved. The reason for this is because communicable diseases have been at the top as a global health priority while non communicable diseases have been at the bottom as a global health priority. The global health system needs to find a way to even out communicable and non communicable diseases. Also, these health problems are heavily framed by private sectors that most of the time benefits from being involved in our global health issues. At the same time, many of these decisions, regarding health problems, are made by industries who emphasize on technological solutions. Governments of all nations need to focus more on proactive solutions rather than relying on private actors to do the job, which they do only to their advantage.[18] Simultaneously, global health policy making is increasingly aligned with industrial and trade policies, and is being done hand in hand with business, thus weakening the firewalls necessary for effective regulation and normative actions both at national and global levels.[18] Many nations have implemented major initiatives to cut smoking, such as increased taxation and bans on smoking in some or all public places. Proponents argue by presenting evidence that smoking is one of the major killers in all developed countries, and that therefore governments have a duty to reduce the death rate, both through limiting passive (second-hand) smoking and by providing fewer opportunities for smokers to smoke. Opponents say that this undermines individual freedom and personal responsibility (often using the phrase nanny state in the UK), and worry that the state may be emboldened to remove more and more choice in the name of better population health overall. However, proponents counter that inflicting disease on other people via passive smoking is not a human right, and in fact smokers are still free to smoke in their own homes.
There is also a link between public health and veterinary public health which deals with zoonotic diseases, diseases that can be transmitted from animals to humans. (See also Vector control).
[edit] Application of Public Health Principles to Healthcare
As well as seeking to improve population health through the implementation of specific population-level interventions, public health professionals also seek to improve population health by improving the contribution of medical care to life extension and quality of life.[19]
Such improvements could be identified by assessing what need for health services existed within the population, and:[20]
1. Assessing current services
2. Ascertaining requirements as expressed by professionals, public and other stakeholders
3. Identifying the most appropriate interventions
4. Considering the effect on resources
5. Agreeing and implementing any necessary changes
In addition public health professionals can improve population health through:
1. Assessing evidence of effectiveness and cost-effectiveness for proposed interventions
2. The evaluation of healthcare to determine whether the activity in question is meeting its objectives[21]
3. Supporting decision making in healthcare and planning health services[22]
[edit] See also
- Behavioral medicine
- Global health
- Global Mental Health
- Health care delivery
- Health profession
- List of preventable causes of death
- National public health institutes
- Universal health care
[edit] Notes
- ^ C.-E. A. Winslow, 'The Untilled Fields of Public Health,' Science, n.s. 51 (1920), p. 23
- ^ WHO Definition of Health Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference, 1946
- ^ http://www.globalhandwashing.org/Publications/Lit_review.htm
- ^ The Solid Facts: Social Determinants of Health edited by Richard Wilkinson and Michael Marmot, WHO, 2003
- ^ a b c d e Patel, Kant; Rushefsky, Mark E.; and McFarlane, Deborah R. The Politics of Public Health in the United States, M.E. Sharpe, 2005, p. 91. (ISBN 076561135X)
- ^ Fee and Acheson, A History of education in public health: Health that mocks the doctors' rules, OUP, 1991. (ISBN 0192617575 )
- ^ Brandt, A. M., and M. Gardner. 2000. Antagonism and Accommodation: Interpreting the Relationship Between Public Health and Medicine in the United States During the Twentieth Century. American Journal of Public Health 90:707 ' 715.
- ^ White, K. L. (1991). Healing the schism: Epidemiology, medicine, and the public's health. New York: Springer-Verlag.
- ^ a b http://www.cdc.gov/mmwr/PDF/wk/mm4850.pdf
- ^ "Schools of Public Health and Public Health Programs". Council on Education for Public Health. 19 November 2009. http://www.ceph.org/files/public/Master_List.v.11.pdf. Retrieved 12 January 2010.
- ^ ASPH
- ^ http://www.ceph.org/i4a/pages/index.cfm?pageid=1
- ^ http://www.deltaomega.org/
- ^ European Union Public Health Information System - HIV/Aides page
- ^ European Union Public Health Information System - Diabetes page
- ^ The Lancet, Volume 375, Issue 9733, Page 2193, "Type 2 diabetes'time to change our approach" 26 June 2010
- ^ European Union Public Health Information System - Smoking Behaviors page
- ^ a b Ollila, Eeva (22 April 2005). "Global health priorities ' priorities of the wealthy". Global Health 1 (6): 6. doi:10.1186/1744-8603-1-6. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1143784/.
- ^ Gillam Stephen; Yates, Jan; Badrinath, Padmanabhan. Essential Public Health. Cambridge University Press 2007.
- ^ Pencheon, David; Guest, Charles; Melzer, David; Gray, JA Muir. Oxford Handbook of Public Health Practice. Oxford University Press 2001.
- ^ Smith, Sarah; Sinclair, Don; Raine, Rosalind; Reeves, Barnarby. Health Care Evaluation (Understanding Public Health). Open University Press 2006.
- ^ Sanderson, Colin; Gruen, Reinhold. Analytical Models for Decision Making (Understanding Public Health). Open University Press 2006.
[edit] References
- Breslow, Lester, ed (2002). Encyclopedia of Public Health. New York: Macmillan Reference USA. ISBN 9780028653549. OCLC 469905883.
- Heymann, David L., ed (2008). Control of Communicable Diseases Manual. Washington, D.C.: American Public Health Association. ISBN 9780875531892. OCLC 232981417.
[edit] External links
| Wikimedia Commons has media related to: Public health |
- Public Health Information Network at the U.S. Centers for Disease Control
- Public Health Agency of Canada
- The official Public Health Portal of the European Union
- Healthy Stories - a collection of stories concerning public health
- public health
|
SOURCES.COM is an online portal and directory for journalists, news media, researchers and anyone seeking experts, spokespersons, and reliable information resources. Use SOURCES.COM to find experts, media contacts, news releases, background information, scientists, officials, speakers, newsmakers, spokespeople, talk show guests, story ideas, research studies, databases, universities, associations and NGOs, businesses, government spokespeople. Indexing and search applications by Ulli Diemer and Chris DeFreitas.
For information about being included in SOURCES as a expert or spokesperson see the FAQ . For partnerships, content and applications, and domain name opportunities contact us.
